What is breech?
Breech means that your baby is lying bottom or feet first in your womb (uterus) instead of the lying in the headfirst (cephalic) position. Earlier in pregnancy breech presentation is very common, however by 36-37 weeks most babies will naturally turn into the headfirst position.
Towards the end of pregnancy approximately 3 to 4 in 100 (3-4%) of babies will be in the breech position.
Why is my baby breech?
It maybe by chance that your baby is in the breech position as opposed to the headfirst position. However, there are certain factors in pregnancy which can make it difficult for your baby to turn making the baby more likely to stay in the breech position. These include:
- Multiple pregnancy
- First pregnancy
- If your placenta is in a low-lying position (also known as placenta praevia)
- If you have little or too much amniotic fluid around your baby
What if my baby is breech at the end of pregnancy?
If at 36 weeks your baby is found to be breech by the use of an ultrasound scan then your midwife or obstetrician will discuss the following options with you:
- Planned elective cesarean section
- Procedure whereby the baby can be turned by a trained professional in the womb (ECV)
- Planned vaginal breech birth
What is External Cephalic Version (ECV) & what does is involve?
A vaginal breech birth can be more complicated than a vaginal birth where the baby’s head is first, therefore your obstetrician or midwife may advise trying to turn your baby into the headfirst position. This is called ECV. This is when firm pressure is applied to your abdomen to encourage the baby to move into the headfirst position.
The procedure is carried out within the Pregnancy Assessment Unit (PAU) with a trained obstetrician and midwife in attendance. Following a discussion of the risks and benefits, you will be asked to sign a consent form prior to the procedure.
The procedure is usually carried out between 36- and 39-weeks’ gestation; however, it can be carried out right up until the early stages of labour.
You do not need to make any preparations prior to an ECV.
You will be given a medication called Terbutaline, via a small injection into your arm to relax the muscles of the uterus as this has been shown to make the procedure more successful. The medication is safe for you and your baby. It may make you feel flushed and that your heart is beating faster however this will only be for a short period.
Prior to the ECV taking place you will have:
- a Cardiotocography (CTG) to ensure the wellbeing of your baby,
- your blood pressure & pulse measured
- an ultrasound scan to determine the exact position of your baby.
Once the position of your baby is determined then the procedure will start. The practitioner may apply gel to your abdomen, and then they will apply firm pressure in order to move the baby into the desired position. This can be uncomfortable but shouldn’t be painful. If it is, then you should ask the person carrying out the procedure to stop or ask the midwife in attendance with you to ask them to stop.
Your baby will then be monitored using the CTG post procedure, whether the procedure is successful or not.
The whole process may last up to 90 minutes, this includes the time taken to administer the medication and monitoring both before and after the ECV. The procedure itself lasts between 5-10 minutes however this can vary person to person.
Does ECV always work?
ECV works in approximately 50% of cases. However, your obstetrician will give you your own individual chance of success based on your clinical situation and their assessment of your pregnancy.
If your baby does not turn and the ECV is unsuccessful then your obstetrician will discuss the next options with you following the ECV or in the antenatal clinic if deemed appropriate.
If you have a successful ECV then there is a small chance your baby will turn back into the breech position. This is less than a 5 in 100 (5 %) chance for women who have had a successful ECV.
ECV should not be carried out if:
- You need a caesarean section for other reasons, such as placenta praevia
- You have had recent vaginal bleeding
- Your baby’s heart rate tracing (CTG) is abnormal
- Your waters have broken
- You are pregnant with more than one baby
Risks involved when having an ECV?
ECV overall has a very low complication rate.
Immediately after ECV there is a 1 in 200 (0.5%) risk of needing an emergency caesarean section due to bleeding from the placenta or changes in the baby’s heartbeat. We therefore carry out a CTG for 30mins after the procedure to check that baby’s heartbeat.
The membranes may rupture (waters break) during the procedure.
If you are Rh negative blood group evidence suggests the risk of fetomaternal haemorrhage (where mum’s and baby’s blood can mix) is 2.4%. You will be provided with an injection of Anti D post ECV to cover you for this.
At home after an ECV
You should telephone the Pregnancy Assessment Unit if you have any vaginal bleeding, abdominal pain, contractions, reduced fetal movements or if your waters break following an ECV.
You can call the Pregnancy Assessment Unit on 0191 445 2764 any time of the day, seven days a week.
Is there anything else I can do to help my baby turn?
There is no scientific evidence that lying down or sitting in a certain position can help your baby to turn. There is some evidence that the use of moxibustion (burning a Chinese herb called mugwort) at 33-35 weeks gestation may help your baby turn. This should be performed under the direction of a registered practitioner.
What is my ECV is unsuccessful?
If your ECV is unsuccessful your obstetrician may offer you another attempt at ECV on a different day. If your baby remains breech then you will be referred to Antenatal clinic or PAU to have a full-informed discussion with an obstetrician. The following options are open to you:
- Planned elective cesarean section
- Vaginal breech delivery
Caesarean section
If your baby remains breech you will be offered the option to have an elective caesarean section. This will involve being given a date and time to attend the labour ward on your allocated day to have your surgery. 2-3 days prior to your surgery you will be given a date and time for a preoperative assessment where you will have bloods and swabs taken, see a member of the anesthetic team and discuss and sign your consent form if it is not already done.
Current research suggests that that caesarean section is a safer way to deliver a breech baby; however, a cesarean section can carry a slightly higher risk for you as the mother.
Please see our leaflet on planned (elective) caesarean section for further information.
Vaginal breech delivery
Prior to going ahead with a planned breech vaginal delivery, you should have had a full informed discussion with your obstetrician with regards to your suitability for a vaginal breech and the risks and benefits involved.
Induction of labour is not generally recommended.
Vaginal breech labour carries a 40% chance of requiring an emergency caesarean section.
Vaginal breech birth carries a reduced risk for you as the mother, however, it does carry a small increased risk to your baby’s survival around the time of delivery. Vaginal breech birth may cause serious short-term complications for your baby. However, these complications do not seem to have any long-term effects on your baby.
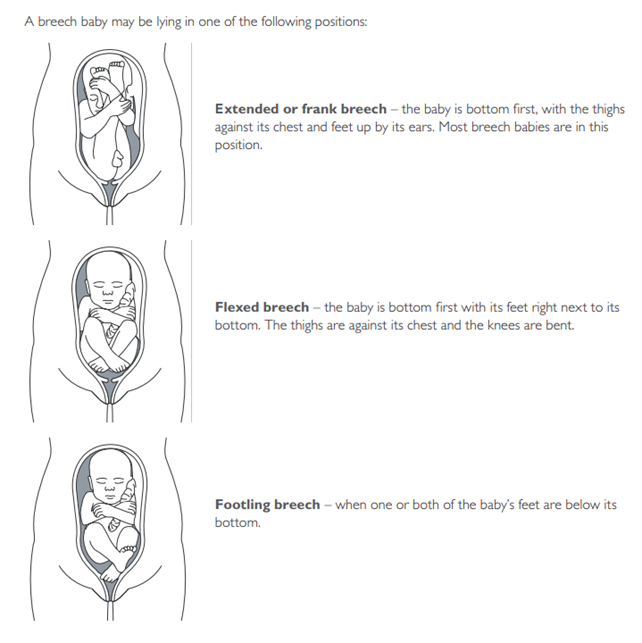
Your obstetrician may advise you against a vaginal breech for the following reasons:
- Your baby is a footling breech
- Your placenta is low lying (covering the opening where the baby would come out)
- Your baby is larger or smaller than we would expect
- If your baby’s head is tilted back (hyperflexed)
Useful sources of information
1. Tommy’s PregnancyLine: 0800 0147 800
2. Bliss (for babies born premature or sick) www.bliss.org.uk
3. Support email: [email protected]
At the Queen Elizabeth Hospital Maternity Unit, we advocate a shared decision-making approach to all decisions made by our patients. This leaflet aims to give you additional information and to act as a point of reference following a discussion with your obstetrician or midwife. If you are asked to make a decision about your own care please make sure you have asked all the questions you need to ask and are given the appropriate time to do so. Some questions you might want to ask could be;
- What are my options?
- What are the pros and cons of each option?
- Who will support me making the decision that is the right one for me
Contact Number
If you have any additional queries please contact:
Your Community Midwife on:
0191 445 5306 (08:30-16:30)
The Pregnancy Assessment Unit on 0191 445 2764 (24 hours)
Delivery Suite on 0191 445 2150 (24 hours)