The information has been compiled to try and answer some of the questions you and your family may have about breast cancer and its treatment. You will be fully involved in any decisions about your care and treatment. Your breast care nurse will be able to give you further information or advice.
Breast Care Nurse (BCN)
After diagnosis, you will be allocated a breast care nurse/key worker and given a contact card with her details on. The breast care nurses work as part of the breast team. They are a qualified nurse who has specialist training in breast care. Your breast care nurse can provide practical information and support.
If you are unable to contact your BCN for any reason, you can contact the hospital switchboard on 0191 4820000 and ask them to transfer you to your breast care nurse’s answer machine where you can leave a message and she will return your call as soon as possible.
The best time to contact your breast care nurse is 9.30 – 4.30pm Monday to Friday
Please note that when your breast care nurse contacts you it will be a withheld number.
You can obtain further free information from:
Cancer BACK-UP / Macmillan Support
Breast Cancer Now
What is breast cancer?
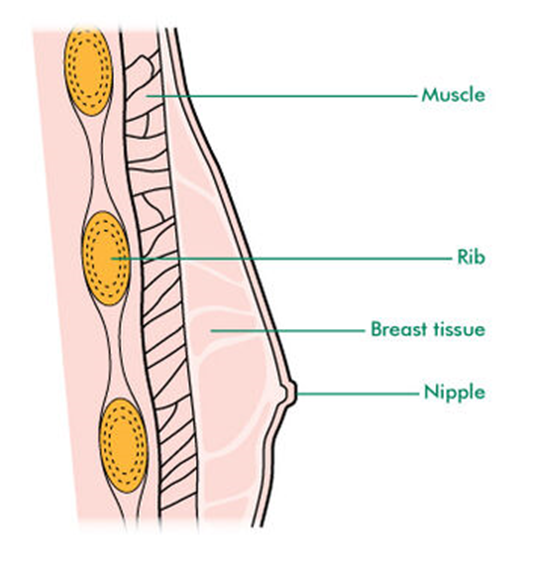
Breasts are made up of many glands, which are lined by tiny building blocks called cells. Normal cells reproduce; repair and when they become worn out, die and new cells are produced to replace them.
Sometimes this process gets out of control and the cells continue to divide, developing a lump which is called a tumour. In some women it can take up to three or four years for a tumour to appear. Tumours can be either benign (not cancer) or malignant (cancer). The majority of breast lumps are benign and cannot spread. Malignant tumours are made up of cancer cells, which may develop the ability to spread to other parts of the body through the blood or lymphatic system.
Other signs and symptoms include:
- A change in shape, size or skin texture of the breast
- Puckering or dimpling of the skin
- Discharge from the nipple
- Your nipple drawing inwards (inversions)
- Soreness or redness of skin around the nipple
There are many different types of breast cancer but we may not know much about your type of cancer until after your surgery. Your surgeon or nurse will be able to give you more information about this after your surgery.
Breast cancer in men
Male breast cancer is rare. Men have breast tissue behind the nipple. This is where breast cancer may develop. It usually happens in men over 60 but can occasionally affect younger men.
Common types of breast cancer
Breast cancer can either be invasive or non-invasive (also described as ‘in situ’). Invasive breast cancer has the potential to spread to other areas of the body. Non-invasive breast cancer has not yet developed the ability to spread to other parts of the body.
Ductal carcinoma in situ (DCIS)
Ductal carcinoma in situ (DCIS) is an early form of breast cancer, sometimes described as intra-ductal or non-invasive cancer. This means that the cancer cells are inside the milk ducts (in situ) and have not yet developed the ability to spread either outside the ducts into surrounding breast tissue or to other parts of the body.
There are different grades of DCIS. If DCIS is left untreated, the cells may eventually develop the ability to spread and it can become an invasive cancer.
As DCIS does not usually have noticeable symptoms (although it may present as a lump) it is most commonly diagnosed from a mammogram (breast x-ray). DCIS is less common in men that in women.
Invasive ductal breast cancer
Most breast cancers fall into this category. With invasive ductal cancer, the cancer cells are no longer confined to the breast ducts. They have spread outside the ducts to the surrounding breast tissue.
Invasive lobular breast cancer
Invasive lobular breast cancer occurs when cancer cells in the lobules (milk-producing glands) have begun to spread outside the lobules and into the breast tissue. Invasive lobular breast cancer is generally no more serious than other types of breast cancer. However, it behaves differently to other types of breast cancer and is sometimes found in more than one area of the same breast, or occasionally in both breasts at the same time. Having breast cancer in one breast means there is a very slightly higher risk of developing cancer in the opposite breast compared to someone who has never had breast cancer. With invasive lobular breast cancer, this risk may be slightly higher than with other types of breast cancer, but is still very low overall.
This type of cancer is rare in men as men have very few lobules in their breasts.
Paget’s disease of the breast
Paget’s disease of the breast is another type of breast cancer that first shows as changes to the nipples. Paget’s disease of the breast is not the same as Paget’s disease of the bone. Paget’s disease is rare in men.
Medical and nursing training
It would be impossible to train future members of the health profession without the help and co-operation of patients. This is a Trust which provides training for medical and nursing students. Students can often be attached to the medical team which will be treating you.
During the process of your treatment, you may be asked whether you would be willing to take part in a teaching session attended by a medical student or junior staff. If you do not wish to take part in any teaching work, you can refuse without your treatment being affected in any way. In this case, you should inform your BCN or the doctor as soon as possible.
The multidisciplinary team
The multidisciplinary team (MDT) is a team of specialists who meet regularly to discuss patient’s treatment plan. The team meets every Monday at 8.00am in the Breast Screening Unit. The whole team is involved through formal discussions in any decisions made regarding your care. Although you are unable to attend these meetings, your views regarding your care will be taken into account during discussions. Your consultant/breast care nurse will inform you of any treatment plan regarding your care. This process will ensure that all patients have the benefit of expert advice.
This team may consist of:
Breast surgeon
A doctor who removes cancer by surgery.
Breast care nurse specialist
A registered nurse who has received additional training in breast cancer.
Radiographer
Person trained to perform and read mammograms.
Radiologist
A doctor who uses scans and x-rays to investigate and diagnose conditions.
Histopathologist
A doctor who has trained to look at tissue samples to determine a diagnosis.
Oncologist
A doctor who specialises in treating patients with radiotherapy, chemotherapy and hormonal therapy.
Your treatment plan
The choice of treatment you receive should be made jointly by you and your specialist following the advice from the team meeting discussion. You should ask what all your options are and their potential risks, benefits and implications for further treatments. The options that have been discussed with yourself and the surgeon are:
Surgery â–¡
Radiotherapy â–¡
Chemotherapy â–¡
Endocrine therapy â–¡
Herceptin â–¡
NEO-Adjuvant Chemotherapy â–¡
Other –
Surgery is usually the best way of treating early breast cancer. However, although there are other treatments available, these may not be as effective if they are not combined with surgery and they also have risks and side effects.
Your treatment plan will be discussed at the breast multidisciplinary team meeting. It may be advised that you have chemotherapy before you have your surgery. This will be discussed with you by your consultant or breast care nurse. If you wish to have a copy of the letters of the discussions you have had with your surgeon please ask for a copy.
Treatment Options
Some patients will be given a choice of which surgery to have, either a Lumpectomy (wide excision/breast conservation) or a Mastectomy.
Here are some of the things that are taken into consideration when making a decision.
Mastectomy
Advantages:
- You do not usually need radiotherapy.
- Some patients find it easier to cope with having all their tissue removed.
- You may be able to have a reconstruction at the same time or at a later date.
- There will be less possibility of further surgery.
Disadvantages:
- It may be more difficult to cope with the loss of the whole breast.
- You may have difficulties dealing with changes to your body image.
Lumpectomy (Wide local excision)
Advantages:
- You will have a smaller scar.
- You will still have the majority of your breast tissue.
Disadvantages:
- You will usually need to attend for radiotherapy treatment.
- You may worry about still having breast tissue.
- You may have discomfort due to surgery or radiotherapy.
You do not have to rush to make a decision. Your breast care nurse will discuss your options with you.
Your reaction to your diagnosis
The diagnosis of breast cancer can be a shock and it can be hard to take in. Even when the diagnosis has sunk in it is normal to carry on feeling distressed. Common reactions include low mood and depression, as well as fear and anxiety about what lies ahead. Family and friends may also be upset.
It is important that you get the right kind of support at this difficult time. Your breast care nurse will be able to support you and put you in touch with other parts of the Breast Service which offer support as well. Most patients find that they do cope with the experience of cancer with the right support from family, friends and the Breast Care Team. For some patients, counselling or psychological help can provide the extra support they need to be able to cope.
If you feel that you might benefit from this kind of support, talk to your breast care nurse who can refer you.
Psychological help in breast cancer is a dedicated service which is not part of Mental Health Services. It aims to help patients cope as well as they can with real difficulties.
Holistic assessment
What is holistic assessment?
Holistic assessment is a discussion with a healthcare professional (usually your breast care nurse), about your physical, social, spiritual and psychological needs. It gives you an opportunity to think about your needs after being diagnosed with breast cancer and agree a plan to meet these needs.
What does holistic assessment involve?
The assessment involves a discussion with your nurse about your needs/concerns and the completion of a written assessment. Your nurse will assess some of your needs during your discussions with her at various stages. If you wish to discuss your concerns/needs in more detail, complete the form provided and give it to your nurse and she can discuss this with you.
This self-assessment is optional; however, it will help us understand the concerns and feelings you have. It will also help us identify any information and support you may need in the future.
If any of the problems below have caused you concern in the past week and if you wish to discuss them with a health care professional, please tick them and make your breast care nurse aware that you have completed this.
Holistic Assessment
Please tick all that apply
| Social | Physical | ||
| Coping with dependants | Difficulties communicating | ||
| Work hobbies/leisure | Sleep | ||
| Finances | Pain | ||
| Parking/travel | Hot flushes and sweats | ||
| Support | Tiredness/fatigue | ||
| Psychological | |||
| Anxiety | |||
| Depression | |||
| Fear | |||
| Body image issues | |||
| Stress |
Your plan of care over the next few weeks
You will need to attend the hospital for various appointments over the next few weeks. Here is a check list of what appointments you may require. Your breast care nurse will discuss this with you.
- Appointment at the breast unit for further biopsies or further scans
- Appointment with your surgeon for further results
- Pre-assessment appointment (you will receive a letter with the admission details and nil by mouth time)
- Appointment for Radioactive injection
- Appointment for RFID tag
- Your operation date
- Appointment with the breast care nurse for wound care if required
- Appointment with surgeon for your results
What happens now?
You will be invited for a pre-assessment. This visit gives the pre-assessment team time to examine you and to arrange any further tests that may be necessary.
These may include blood tests, a chest x-ray, and possibly a tracing of your heart (ECG or echocardiograph). None of these are painful and they are all routine before any operation. You will need to attend the pre-assessment department for up to one hour.
What happens when I am admitted to hospital?
You will be asked to attend the Day Unit on your own unless you need a carer. The anaesthetist will visit you before the operation and your doctor may also see you. Please ask them any questions at this point, it is important you understand what is going to happen.
Shortly before your operation you will be asked to undress and put on a cotton operation gown. It is advisable to wear cotton underwear under your gown. You will need to remove contact lenses and all jewellery except your wedding ring. You will then be taken to the theatre where you will be given an injection to send you to sleep before the operation begins.
Radio Frequency Identification tag (RFID tag)
Some patients require a RFID tag before their surgery to help the surgeon to locate your cancer. If you require this your surgeon will discuss this with you.
What is TAG localisation?
TAG is a procedure used when an area of breast tissue that needs to be removed cannot be felt by examination, and the surgeon needs a guide to ensure he removes the correct piece of tissue during surgery. A TAG is a tiny radiofrequency device (smaller than a grain of rice) that can be inserted into the breast tissue by the radiology team (a doctor or other trained professional who specialises in x-ray) while you have an ultrasound scan or mammogram. The procedure can be done up to 30 days prior to your surgery. It will involve attending the breast screening unit as an outpatient.
What are the benefits of TAG localisation?
TAG insertion allows location of the breast tissue that needs to be removed several days before surgery.
What are the alternatives to TAG localisation?
The alternative method to this procedure is a guidewire procedure which involves inserting a small fine wire into your breast under ultrasound/mammogram which will then be a guide to the surgeon when he/she removes the tissue. This would need to be done on the day of your surgery. Patients sometimes find the guidewire uncomfortable and this procedure can increase anxiety on the day of surgery.
What does the procedure involve?
The TAG is inserted by the radiologist or other qualified member of the breast team (a radiographer). The procedure is similar to the core needle biopsy you will have had to your breast that confirmed your diagnosis. You will attend the breast unit and have an ultrasound scan or mammogram of your breast to locate the cancer. The radiologist or radiographer will then inject a local anaesthetic (numbing medicine) into your breast. This may sting for a few seconds but will numb your breast quickly. The radiologist or radiographer will then use a small thin needle to place the TAG into the area of cancer that needs to be removed. You may feel some pressure in your breast during the procedure but this is not normally painful. If you do feel any pain, please make the staff aware so that more local anaesthetic can be given. You will not be able to feel the TAG once it is inserted and you can continue with your normal activities. A small dressing will be placed over the puncture site. The procedure will usually take about 30 minutes.
What are the risks of TAG localisation?
You may have some mild discomfort and bruising. If you do have discomfort or pain then you can take your regular pain relief.
You may have a small amount of bleeding on your dressing. This is normal. If you have any heavy bleeding that soaks through your dressing apply firm pressure. If this continues and you are concerned you can contact your breast care nurse.
If you have any signs of infection, such as a high temperature or redness, then contact your breast care nurse.
What happens after the TAG localisation?
You can remove the dressing after 24 hours. You can return to work and most activities the following day. Avoid heavy lifting for 24 hours. You may shower the following day but do not soak in a bath or go into a swimming pool for 48 hours. It is recommended that you wear a comfortable supportive bra for 24 hours.
What happens during surgery?
During surgery while you are asleep under general anaesthetic, the surgeon will use a highly sensitive detector to identify the TAG and location of the breast tissue that needs to be removed. The surgeon will then proceed with your surgery. The TAG will be removed during surgery.
Wide Local Excision/lumpectomy (Breast Conserving Surgery)
What is Wide Local Excision/lumpectomy or Conservation Surgery?
This is the term used when a breast cancer, plus an area of surrounding tissue, is removed without removing the whole breast. As well as the surgery to the breast, some of the lymph glands in the axilla (armpit) are usually removed. Your consultant may discuss Sentinel lymph node biopsy (see section on Sentinel lymph node biopsy). You may have one or two wounds depending on the location of your cancer. This is done to give further information to the breast team looking after you, to enable them to work out an individual package of care for you.
Why do I need this operation?
You will have had investigations carried out previously and the results of these will have been fully discussed with you by your surgeon, who will have given you full information for you to make a choice of the operations recommended. It is important that you discuss this fully with your surgeon. The breast care nurse will consider your views and encourage you to be involved in making the decision. A breast care nurse specialist will be involved if you require any further information.
What is done during the operation?
You may have one or two incisions. Some patients may have a drain in place. This is a long, thin plastic tube connected to a clear plastic bag or bottle and is secured by a stitch. Some patients may not have any tubes. This tube takes away any excess fluid and blood from your wound, which reduces swelling, pain and allows your wound to heal effectively. The wound is closed together with stitches under the skin. These stitches do not need to be removed as they are made of a dissolvable material and slowly dissolve away.
What happens after the operation?
In the first 24 hours you will be encouraged to move around.
If you have a drain, it will be removed before you go home. When it is time for the drain to be removed the nurse will cut the small stitch, the tube is then slowly removed. You may feel a tugging, uncomfortable sensation but this is only brief, and painkillers can be given afterwards if you experience soreness.
You may be discharged with a support vest on, this is to reduce bruising. This should remain on for at least 48 hours, then it can be removed if you are uncomfortable.
How long will I be in hospital?
Most patients will have surgery as a day case. If you need to stay in hospital it will usually be just for one night, depending on recovery.
When will I get my results?
You will be given an appointment to come back to the clinic in 10-14 days for your results.
A small number of patients may need further surgery. This will be discussed with you when you return for your results.
Mastectomy
What is a Mastectomy?
A mastectomy is an operation to remove all or nearly all of the breast tissue including the nipple. When it is carried out to remove cancer, it is usual that some of the lymph glands in your axilla (armpit) are removed at the same time. This will give the breast team looking after you further information, to enable them to work out an individual package of care for you. Your consultant may discuss Sentinel lymph node biopsy with you (see section on Sentinel lymph node biopsy).
Why do I need this operation?
You will have had investigations carried out previously and the results of these will have been discussed with you by your surgeon who will have given you full information for you to make a choice of the operation recommended. It is important that you discuss this fully with your surgeon. He/she will consider your views and encourage you to be involved in making the decision. A breast care nurse Specialist will be involved if you require any further information.
You have the choice to involve your partner, relative or friends at any consultation. Write your questions down and don’t be afraid to ask them, your surgeon and breast care nurse will be happy to answer your queries.
Can I have a Nipple reconstruction?
Nipple reconstruction may be a suitable option for some patients. Your surgeon/breast care nurse can discuss this with you in more detail.
What is done during the operation?
You will usually have one incision. You may have a drain in place. This is a long, thin plastic tube connected to a clear plastic bottle and is secured by a stitch. This tube takes away any excess fluid and blood from your wound; this reduces swelling and pain and allows your wound to heal effectively. When it is time for the drain to be removed the nurse will cut the small stitch, the tube is then slowly removed. You may feel a tugging, uncomfortable sensation but this is only brief and painkillers can be given after if you experience soreness. The wound is closed together with stitches under the skin. These stitches do not need removing as they are made of dissolvable material and slowly dissolve away.
What happens after the operation?
In the first 24 hours you will be encouraged to move around. You may be discharged with a support vest. This is to reduce bruising. This should remain on for at least 48 hours, then it can be removed if you are uncomfortable.
How long will I be in hospital?
Your stay in hospital after your operation can be as little as 24 hours or 2 days.
When will I get my results?
You will be given an appointment to come back to the clinic in 10–14 days for your results.
Nipple reconstruction
If you are about to have a mastectomy, or have had one in the past, you may now be considering nipple reconstruction. It is important to discuss with the doctor and breast care nurse what options are available and appropriate for you. Delayed reconstruction can take place at a later date – when you feel ready and have had more time to make a decision.
Nipple/areola tattoo; this can be done following your reconstruction.
Prosthesis
Following a mastectomy, you may want to consider a prosthetic nipple. These are made of soft silicone that are either self-sticking or come with special skin glue. Prosthetic nipples come in different sizes and skin colours. Prosthesis can be renewed every two years.
If this is something you would like to consider contact your breast care nurse.
Axillary node biopsy/Axillary node dissection
What is axillary node biopsy/axillary node dissection?
This is the term used when some of your lymph nodes in your axilla need removal and examination by the Histopathologist.
Why do I need this operation?
You will have had investigations carried out previously and the results of these will have been discussed with you by your Surgeon who will have given you full information for you to make a choice of the operation recommended. It is important that you discuss this fully with your Surgeon. He/she will consider your views and encourage you to be involved in making the decision. A breast care nurse Specialist will be involved if you require any further information.
You have the choice to involve your partner, relative or friends at any consultation. Write your questions down and don’t be afraid to ask them. Your Surgeon and breast care nurse will be happy to answer your queries.
What is done during the operation?
You will usually have one incision. You may have drains in place. These are long, thin plastic tubes connected to a clear plastic bag or bottle and is secured by a stitch. This tube takes away any excess fluid and blood from your wound, this reduces swelling and pain and allows your wound to heal effectively. The wound is closed together with stitches under the skin. These stitches do not need removing as they are made of dissolvable material and slowly dissolve away. During your operation you will have a small needle put into your vein to enable you to have intravenous fluids which will prevent dehydration until you feel like eating and drinking – normally within 24 hours.
What happens after the operation?
In the first 24 hours you will be encouraged to be mobile. Your intravenous drip will be removed, providing you are tolerating fluids and diet. The drain, if you have one, will be removed before you go home.
When it is time for the drain to be removed the nurse will cut the small stitch, the tube is then slowly removed. You may feel a tugging, uncomfortable sensation but this is only brief and painkillers can be given after, if you experience soreness.
How long will I be in hospital?
Your stay in hospital after your operation can be as little as a day or two days.
When will I get my results?
You will be given an appointment to come back to the clinic in 10 to 14 days for your results.
Sentinel Lymph Node Biopsy
What is the sentinel node?
The armpit contains lots of small structures called lymph nodes. These are often better known as ‘glands’. Their main job is to help us deal with infections, but may also become involved in the spread of some cancers, and can also become enlarged if this happens. The sentinel node is the first lymph node in your armpit to which breast cancer can spread. The sentinel node is connected to the other lymph nodes in the armpit.
What is a sentinel lymph node biopsy?
A sentinel lymph node biopsy is the removal of the sentinel lymph node. Traditionally women undergoing surgery for breast cancer usually have 4 to 10 lymph nodes removed from the armpit (axilla) at the same time as your operation. By just removing the sentinel lymph node, at the same time as your breast operation we can find out whether or not the breast cancer has spread to your lymph nodes in your axilla. This helps us to advise you about the stage of your cancer and the best type of breast cancer treatment for you.
Side effects of traditional armpit surgery
For some patients, traditional lymph node removal (4 to 10 lymph nodes) can cause temporary shoulder stiffness, nerve pain and one third of patients may develop lymphoedema (swelling of the arm). The side effects of armpit surgery increase with the number of nodes removed. This means if we remove only the sentinel node (usually one or two nodes) side effects are less than traditional armpit surgery where four or more nodes are removed.
Before Surgery
On the day prior to your surgery, you will be given an injection that contains a small amount of radioactivity. This injection is given just under your skin into your breast using a very fine needle; you may feel a stinging sensation, but this should not be too unpleasant as only a tiny volume of liquid is given. This is done in the Medical Physics department and you may receive an appointment to attend your local hospital for this injection.
In most cases that will be it. Very occasionally, a consultant may request a scan to show the relevant lymphatic drainage from the injection site. If this is the case for you, the pictures will take a maximum of 30 minutes to do and will be performed straight after your injection. You will receive an appointment for this by letter or by phone.
During surgery
(Under general anaesthetic) a blue dye may be injected into the breast. This also travels to the sentinel node. The surgeon, using a special radiation detection probe, can then find the sentinel node which is also blue.
What if we cannot find the Sentinel Nodes?
Occasionally it is not possible to find the sentinel node. If this happens, but only with your permission before the operation, the surgeon during the same operation will remove more nodes to make sure the node which is likely to be the sentinel node is removed.
After surgery
The pathologist examines the Sentinel Node under the microscope. If the sentinel node contains cancer cells it is possible further cancerous nodes are still present in the armpit. For this reason, you may require further armpit surgery to remove as many of the remaining lymph nodes as possible. This will mean coming into hospital again. You will be given an appointment 10–14 days after surgery to see your Consultant for the results and if you need to come into hospital for future surgery, this will be discussed at this appointment.
What are the benefits of Sentinel Node Biopsy as opposed to traditional lymph node surgery?
- Less discomfort and less risk of shoulder/arm stiffness
- Less risk of lymphoedema (see page 28)
- Shorter hospital stay and quicker overall recovery
What are the risks of Sentinel Node Biopsy?
- Blue dye will discolour urine, stools, tears, contact lenses (please remove before surgery) for a few days. The breast skin will be discoloured for up to two years and very occasionally longer. You will also be a grey/blue colour initially after surgery.
- Allergic reaction to the blue dye can occur rarely whilst under the anaesthetic. This can be treated but can (very rarely) be severe.
- Injection of radioactive fluid into the breast may give slight discomfort
- If the pathologist finds the sentinel lymph node/nodes contain cancer, you will need more armpit treatment. This may require a second armpit operation (half of patients) to remove further lymph nodes.
What are the risks/ complications from breast surgery?
Most operations are successful with few complications. However, every procedure has risks and potential complications. Your surgeon will discuss your risks from surgery when he or she consents you for your surgery. Here is a list of the most common complications from breast surgery.
Pain
Pain happens with any operation. You will be given medication to help your pain when you are discharged from hospital.
Bleeding (from the wound)
This can happen during or after surgery. This rarely needs a blood transfusion or another operation but it is common to get bruising of the breast or armpit.
Infection in the surgical wound
If this happens you may need treatment with antibiotics. The wound may need dressing for a few weeks. Very rarely, you may need further surgery. If the skin around the scar is red and your wound is painful inform your doctor or your breast care nurse.
Blood clots (this is a rare occurrence)
Blood clots in the legs (thrombosis), which can occasionally move through the bloodstream to the lungs (embolus). You will be encouraged to move as soon as possible after your surgery to reduce the risk of blood clots.
Disfigurement of the breast (following wide excision)
This will depend on how much tissue the surgeon needs to remove and the size of your breast. Sometimes the breast can swell, particularly if your glands have been removed or after radiotherapy.
Numbness
This is caused by injury to the small nerves that supply the skin. Any pain usually settles after a few weeks. Numbness can last for up to six months and can sometimes be permanent.
Lymphoedema
Lymphoedema is a swelling caused by a build-up of lymph fluid in the tissue. This builds up as a result of damage to the lymph system because of surgery or radiotherapy to the lymph nodes.
- Lymphoedema affects people in different ways. Although swelling of the arm, including the hand and fingers, is the most common symptom, swelling can also affect the breast/chest, shoulder or behind the armpit.
- Your skin may feel stretched, and you might find it more uncomfortable to move your arm. In some people the swelling may result in aching and heaviness.
- It can occur soon after surgery or radiotherapy or it can develop many years later.
- If untreated the lymphoedema can become worse.
- If you develop any swelling of your arm, hand, fingers or around your chest you should report it to your Breast care nurse or Hospital Specialist. You will then be referred to the Lymphoedema Clinic.
- There is a Lymphoedema Clinic at the Queen Elizabeth Hospital run by the Breast care nurses.
- There are also clinics at St. Benedict’s Hospice, Sunderland, St Cuthbert’s Hospice, Durham, St Oswald’s Hospice, Newcastle. You can be referred to any of these clinics if you would prefer.
How can I reduce my risk of lymphoedema?
Not all patients develop lymphoedema. It is not possible to predict which patients will develop this, but the following advice will help to minimise your risk. If you have had Sentinel Lymph Node Biopsy your risk of lymphoedema will be very small. You may be able to reduce your risk by taking the precautions below:
- Treat any scratches, cuts or insect bites promptly with an antiseptic cream
- Use insect repellent
- Avoid injuries by wearing gloves to protect your hands when gardening or washing up
- Use a good protective cream with a high sun protection factor (SPF) when sunbathing to avoid getting sunburnt
- Avoid having blood pressure or blood samples taken from the affected arm. Also avoid injections into the arm
- If you have had a double mastectomy you can have your blood pressure measured and blood samples taken from your legs. If this is not possible then you can use your arms. Discuss this with your nurse.
- Take care when removing unwanted hair from your armpit
- It is very important to maintain good skin condition by applying moisturiser to help prevent infection and therefore reduce the risk of lymphoedema
- If the skin becomes red, hot and tender you must see your doctor immediately. This is a sign of infection and antibiotics may be necessary.
- Use your arm normally, muscle movement encourages lymph drainage and prevents joint stiffness
- Avoid strenuous activities such as pushing or pulling
- Avoid strenuous exercise. Be careful when attending gyms and weight training.
Exercises after breast surgery
It is important to get your arm moving and do arm exercises after your surgery. A typical response to an injury, surgery or to pain is to protect the affected area. This often includes developing a protective posture around the surrounding area/limb and limiting the amount of associated movement. When movement at a joint is restricted for a period of time, the joint can become stiff. Therefore, restricting movement can make the area become more painful.
Increasing pain at a joint is often interpreted as a signal that something is wrong and therefore you may become even more protective of the area, which can cause more problems and cause anxiety.
Exercises
Exercises should start as soon as possible, and you should do them every two hours
When you are awake for the first two weeks and then gradually reduce this.
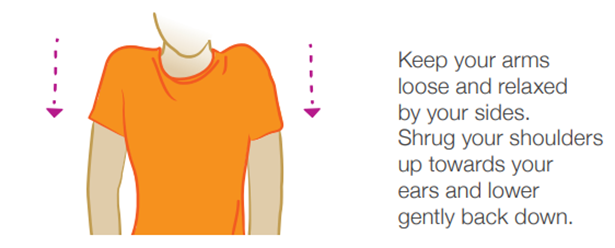
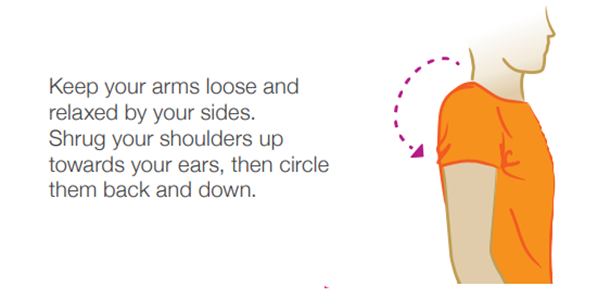
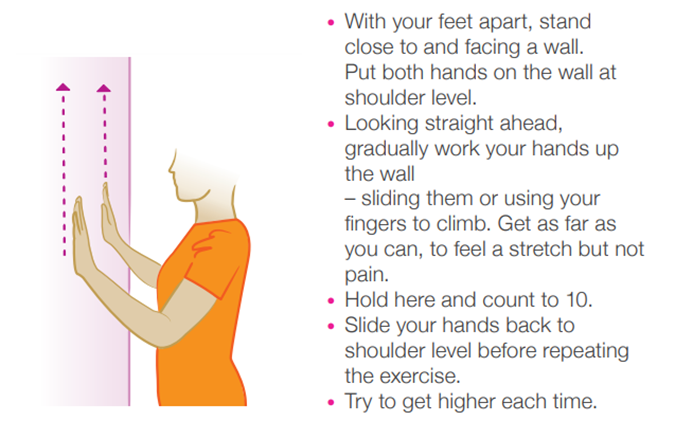
Your breast care nurse can give you further advice regarding exercises.
Post-surgery activities
Below is an easy-to-follow guide on when you can expect to recommence common activities after your surgery. Please remember that everyone is different so this should be used as a guide only. It is important to listen to your body and rest when you need to. If you are unsure about any of the advice here, please get in touch with your breast care nurse.
Post-Surgery activity guide
For wide local excision/lumpectomy or mastectomy with or without sentinel lymph node biopsy
| Activity | Week 1 | Week 2 | Week 3 | Week 4 | Week 5 | Week 6 |
| Walking (slow/mod pace) | Yes | Yes | Yes | Yes | Yes | Yes |
| Arm exercises | Yes | Yes | Yes | Yes | Yes | Yes |
| Sex | Yes | Yes | Yes | Yes | Yes | Yes |
| Light Domestic Cleaning | No | Maybe | Yes | Yes | Yes | Yes |
| Ironing | No | No | Yes | Yes | Yes | Yes |
| Hoovering | No | No | Yes | Yes | Yes | Yes |
| Driving* | No | No | Yes | Yes | Yes | Yes |
| Gentle Exercise (jogging) | No | No | No | Yes | Yes | Yes |
| Carrying Heavy Shopping | No | No | No | Maybe | Yes | Yes |
| Lifting Toddlers | No | No | No | Maybe | Yes | Yes |
| Intense Exercise (running) | No | No | No | No | Maybe | Yes |
*The DVLA recommend that you are able to perform an emergency stop effectively before driving after surgery.
Worries about doing exercise
The drain – drains will not fall out.
The wound – will not break down.
Pain – if you have had your lymph glands removed you are more likely to feel pain and discomfort, particularly in your armpit and running down your arm.
Cording – you may develop a pain which can feel like a tight cord running from your armpit down your arm. This is called cording. It is thought to be due to hardened lymph vessels. It can significantly restrict your arm movements. Stretching exercises can help stretch cords.
Changes in sensation – if you have had your lymph glands removed you may experience the loss of or change in the sensation in your armpit and running down the inside of your arm. This can lead to some of these symptoms:
- Loss or reduced sensation
- Numbness or coldness
- Weakness in the arm
- Sensitivity to touch
- Burning, tingling, pins and needles
These symptoms are usually temporary and improve slowly, but you may be left with some permanent or altered sensation in the armpit or upper arm.
Wound support
Some patients will be fitted with a supportive bodice following surgery. You may keep this on for as long as it is comfortable, you should usually not need this for longer than a week after surgery.
Wound Care
Initially you may be able to bathe and shower as normal provided you have a waterproof dressing. Aim to keep the dressings as dry as possible. After about two weeks you can return to using soaps and toiletries as normal. If you still need a light dressing at this stage then your district nurse, practice nurse or breast care nurse will advise you.
Seroma
Some patients who have had a breast operation will develop a seroma, even if a surgical drain has been used. A seroma is a build-up of bloodstained fluid which can collect under the skin after a breast operation or when the glands have been removed from the axilla (armpit). Small seromas will usually disappear within a month and no treatment is needed. Only if the seroma is large and causing discomfort or problems in using the arm will treatment be needed, in which case the fluid can easily be drained by a doctor or nurse using a fine needle.
For further information please contact your breast care nurse.
General advice after breast surgery
Driving
You may want to wait a couple of weeks until you feel the strength in your arms has returned before you begin driving again. When driving, if your seatbelt starts to cause irritation you can buy an adapter to go on your seatbelt. This will ease the tightness of the belt. These can be bought from car shops.
Please note: It is advisable to check with your motor insurance company following your operation as some companies state a time limit before you can start driving again following an operation. So, it is worth checking to ensure you are legally covered.
Sexual activities
You can resume your sex life as soon as you wish following your breast surgery. Many patients are worried that they will be less masculine and desirable after breast surgery and that their partner will no longer find them attractive. Usually few relationships are affected by this operation. Couples need to talk over their fears and feelings openly and honestly as soon as they feel able after surgery.
Housework
Following your breast surgery, you should be able to return to most of your usual activities within about two to six weeks, but this varies from person to person. Light work can be resumed soon after returning home. Some activities such as ironing or using the vacuum cleaner may take a little longer. It is often easier to start with a small amount of work and gradually increase this.
Lifting
A kettle three-quarters full of water is about the heaviest weight you should lift within the first two weeks after your operation. You will be less likely to feel any discomfort if you use both hands to lift.
Rest
It is important that you set aside time each day to rest. This may be having an early night, late morning or an afternoon nap. Don’t be surprised if you feel tired. As well as having an operation and a general anaesthetic, you have been through a very stressful time, so it is understandable if you feel worn out. Don’t be afraid to take some “time out” for yourself to rest your mind as well as your body.
Sport
Most sports can be resumed after a couple of weeks but please check with your surgeon, breast care nurse and physiotherapist. If your chosen sport involves strenuous upper body movements (for example golf, swimming, aerobics, and racquet sports) then it is probably advisable to recommence these activities gradually about one month after your operation.
Returning to work
You may feel quite tired at first but depending on how you feel and the type of work you do, you may feel able to return to work usually about six to eight weeks after your operation. However, if you need further treatment this may be delayed.
Diet/Exercise
There is a lot of research being done to find out how diet may affect the risk of cancer developing. Some research has shown that being overweight and not eating enough fruit and vegetables could increase your risk of cancer
Eating a balanced diet is one of the best choices you can make for your overall health. Keeping to a healthy weight will help you maintain or regain your strength and have more energy. Regular exercise is also important. More and more research is showing that exercise can reduce the risk of breast cancer coming back (recurrence) if you’ve been diagnosed, as well as reducing the risk of developing breast cancer if you’ve never been diagnosed. Evidence suggests a 30% reduction in risk occurrence. Exercise can also help you maintain a healthy weight, ease treatment side effects and boost your energy. All these steps can also reduce the risk of a new cancer, heart disease, stroke and diabetes.
Making changes to your diet is not always easy. It may be more difficult if you are coping with a cancer diagnosis and having treatment. You could make changes gradually so that it is easier to eat differently. Many people find making this positive choice helps give them back a sense of control. It can also help you feel that you’re doing the best for your health. Thinking about what and how much alcohol you drink is part of this too. Eating well and keeping to a healthy weight will help you maintain or regain your strength, have more energy and have an increased sense of wellbeing.
Following the operation, it is common to feel a lack of confidence. Breast cancer surgery can be a deeply traumatic experience. People find different ways of coming to terms with the change to their bodies. Help is available. No-one has to deal with their experience alone, unless they prefer to do so. Your Breast Cancer Nurse Specialist is an expert in providing support at this time.
The support of a caring partner or close friend can also be invaluable. Talking to other patients who have had breast cancer can also be helpful. Your breast care nurse can arrange this for you.
General advice
It is not uncommon after any form of breast surgery to feel discomfort on movement of the arm and shoulder and some “pulling” down the arm. Gently putting the arm through a whole range of movements as soon as possible after surgery will help to overcome this problem. Exercises should continue for at least six weeks after surgery and for a further six weeks after you have had radiotherapy treatment.
- Your chest may feel tender and tingle. Some people may experience sharp stabbing pains across the scar line or down the arm.
- You may experience some numbness under your arm. This is usually temporary.
- Listen to your body – be gentle with yourself and rest between tasks. Gradually your energy levels will return, try to do a little each day.
- Deodorant may be used under the arm when the wound is completely healed
- Use and hold your arm normally
- Dusting, hanging out washing (if it is not too heavy), washing and drying dishes, cleaning windows and ironing in moderation are all good exercises. However, do not use your vacuum cleaner.
- Try to go out for a walk each day, even if it is around the garden or down the path
- You will be able to drive again when your wound has healed, and your stiches are out. Some extra padding around your seat belt may help you feel more confident if you need to brake sharply.
- You should avoid heavy lifting for the first two weeks.
- Do not walk dogs on a lead on the affected side – they could pull your arm painfully
- You may return to normal sexual activity as soon as the wound feels comfortable
Virtual Wellness Clinic
This is a virtual clinic offered to our breast cancer patients. This clinic is accessed via TEAMS on the computer rather than a face-to-face session and there is support available to access the session and a written guide available. This specialist clinic offers the opportunity to learn about treatments such as chemotherapy, Herceptin, radiotherapy, letrozole and tamoxifen. This will include potential regimes, side effects and timelines for treatment. You will also be given information about benefits and other financial support, learn more about returning to work following treatment, discover information about a good diet and lifestyle and become more knowledgeable about long term side effects and the consequences of treatment. You will also have the opportunity to learn more about issues relating to breast cancer and follow up including surveillance, genetics and body image.
We will also give you the opportunity to talk to other patients who have completed treatments and can give you helpful tips and practical advice about radiotherapy, chemotherapy and endocrine therapy.
If you have any questions about this clinic please contact your breast care nurse.
Movement Recovery and Improvement Programme
The breast team offer a 6-week program to patients currently on or recovering from treatment. The sessions take place on a weekly basis virtually (on a computer, phone, iPad) This programme is accessed via TEAMS on the computer rather than a face-to-face session and there is support available to access the session and a written guide available. Each session is dedicated to an aspect of cancer and is delivered by a professional expert in that field. These sessions are aimed at improving patient knowledge, confidence and promoting peer and social support. Potential topics included in these sessions are managing hair loss, diet and weight management, body image, exercise, lymphoedema, fatigue and finances. If you have any questions about this
6-week programme please contact Caroline Tweedie (breast nurse specialist) on 0191 445 2050.
How to use Microsoft Teams
You can join the session via your mobile phone, tablet, home computer or laptop.
Mobile phone or tablet
If you’re joining from a mobile phone or tablet you will be required to download the Teams app from the Apple App Store or the Google Play Store. Once downloaded, simply click the link in the email to join.
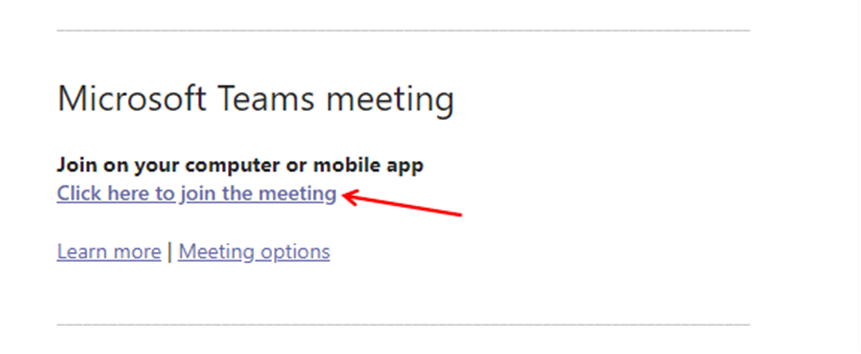
Home computer or laptop
Step 1
Click the link in the invitation email to join.
Step 2
On a home computer or laptop, there are two ways to join a Microsoft Teams meeting, using the Teams app or through your web browser.
If you already have the Teams app installed on your computer, you might get a pop-up asking if you want to open the app. Click ‘Open Microsoft Teams’
If not, you can either download the Teams app, or just use Teams in your browser.
We suggest clicking ‘Continue on this browser’ as it is quicker and does not require the app do be downloaded.
Step 3
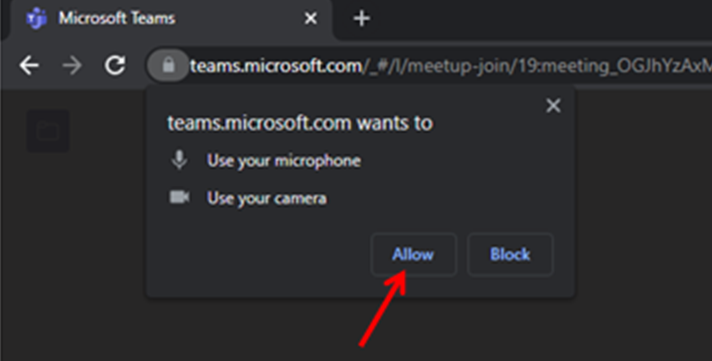
If you’ve never used Microsoft Teams before, chances are you will be asked to allow access to your microphone and camera. You MUST click ‘Allow’ even if you don’t want to share your video. You can turn your camera off in the next step.
If you’re logged into a Microsoft account (Outlook, Office etc.) then you may not be asked to enter your name. If you are prompted, enter the name you would like the rest of the group to see. If you would like to stay anonymous during this session please enter your initials or Anon.
At this point you can also turn off your camera by clicking the slider next to the camera icon.
You can also mute yourself before joining the call by clicking the slider next to the microphone icon.
Alternatively you can ring your breast care nurse.
Podcasts
We have created a series of podcasts (A radio program) offering advice and support that patients can access at their own leisure. We have a host of professionals explaining about different aspects of your care and also patients recapping on their experience of cancer. You can access these through the trust YouTube link, or you can just google ” Queen Elizabeth Gateshead patient podcasts”. Contact your breast care nurse for more information.
You can access our breast podcasts on the following link – Patient cancer podcasts – YouTube
QR Code for Podcasts

To use the QR Code
- Open the QR Code reader on your phone.
- Hold your device over a QR Code so that it’s clearly visible within your smartphone’s screen.
- Two things can happen when you correctly hold your smartphone over a QR Code.
- The phone automatically scans the code.
- On some readers, you have to press a button to snap a picture, not unlike the button on your smartphone camera.
- If necessary, press the button.
- Your smartphone reads the code and navigates to the intended destination, which doesn’t happen instantly. It may take a few seconds on most devices.
- To use the email link
- Open Google and insert the link into the search engine.
- Alternatively, you can google Queen Elizabeth Gateshead Cancer podcasts.
Male breast cancer podcast QR code – Male breast cancer with Oncoplastic Breast Surgeon & Specialist Breast Care Nurse.

What other treatments will I need for my breast cancer?
After your surgery additional treatment for breast cancers are usually required. A number of different treatments are used and include the following:
- Radiotherapy
- Chemotherapy
- Herceptin
- Tablets (endocrine therapy)
The type or types of treatment you require will depend on a number of factors which include the sort of tumour you have had, and whether you have gone through the menopause or not. All this will be discussed in detail when the results of your surgery are known.
Oncotype DX Test
This is a gene test that measures the activity of genes in cancers. These tests can provide useful information where there is uncertainty about the benefit of chemotherapy in helping to prevent breast cancer from returning. Your surgeon/breast care nurse will be able to advise you if you are suitable for this test and give you more information about it if you wish.
Radiotherapy
Radiotherapy is the use of high energy x-rays to kill cancer cells. These cells are more sensitive to radiotherapy than normal cells and they will be destroyed. Normal cells in the treated area are also affected but they can recover quickly. The treatment is painless. It does not make you radioactive and there is no reason not to mix with other people.
Radiotherapy is usually started six to eight weeks after surgery. Treatment usually lasts one to three weeks. You will have to attend everyday Monday to Friday at the Freeman Hospital. Each treatment usually takes approximately five minutes. Your first visit to clinic is called the “planning visit”. Please bring with you any medication you are taking. Marks are drawn onto your skin to indicate the area to be treated. It is important not to wash these marks off until your treatment is finished. Alternatively, very small tattoos can be placed on your skin to mark the treatment field. This planning visit lasts one to two hours.
A special backrest is used to support your arms during treatment. Both arms will need to be positioned above your head. It is important that you exercise your arm appropriately after your surgery to ensure that you regain full movement of your shoulder. If you have any difficulty moving either shoulder you will need to inform your breast care nurse as you may require additional physiotherapy.
If you require transport to take you to the Freeman Hospital, the charitable organisation ‘Daft As A Brush’ can arrange to transport you to and from the Freeman Hospital whilst undergoing treatment. This can be organised once you have seen an oncologist. You can also book a transport ambulance if required.
You may feel very tired during or after your treatment. Side effects of radiotherapy are usually temporary and mainly affect the skin on the area to be treated. Fair to sensitive skins may develop some redness and/or blistering. If you have not had a mastectomy, some swelling of the breast may occur. After the breast has settled down following radiotherapy, it may be slightly smaller than the other breast. If you have any skin problems contact one of the specialist breast radiographers, for advice at Freeman Hospital Tel: (0191) 244 8716. Further information about radiotherapy can be obtained from your breast care nurse or oncologist.
Tamoxifen
Tamoxifen is an anti-oestrogen drug, which is thought to influence the growth of breast cancer cells. Tamoxifen helps prevent new cancer cells from developing and can shrink an existing breast cancer.
You will usually take one 20mg tablet a day at a time which suits you, for 5 or 10 years. Further prescriptions can be obtained from your general practitioner. Do not worry if you occasionally forget the tablet, just take the next one as usual. It may increase the effects of anti-coagulant drugs such as Warfarin.
Other benefits Tamoxifen may have are protection against osteoporosis and reducing the risk of heart disease and strokes.
Tamoxifen is a well tried and effective drug with few side effects. Please find the information leaflet enclosed with your tablets and talk to your pharmacist. Common side effects experienced are:
- Hot flushes or sweats
- Lower sex drive and erection difficulties
- Nausea
- Tiredness
- Weight gain
Aromatase Inhibitor drug therapy e.g., Letrozole, Anastrozole and Exemestane
Hormones are naturally occurring substances which control the growth and activity of normal cells in the body. Examples of such female hormones are oestrogen and progesterone which can also affect the growth of breast cancer cells. It is known that a high level of oestrogen circulating in the body is a risk factor for breast cancer.
These drugs block oestrogen and/or its effects which are used to treat breast cancer, both early and advanced. How they achieve this effect is not yet completely understood. These drugs are used to treat post-menopausal women with breast cancer.
If you are prescribed one of these drugs, you will need to have a DEXA Scan (a scan to check your bone marrow density) as these drugs can cause a reduction in the density of your bone mineral and therefore increase your risk of developing thinning bones. Your consultant will arrange this scan for you.
You will be seen by the Osteoporosis Nurse Practitioner who will give you your result and advice on any medication or lifestyle changes you may require for osteoporosis or prevention.
The DEXA Scan will be repeated at two years and five years. This will be arranged by osteoporosis team.
Chemotherapy
Chemotherapy is the use of anti-cancer drugs to destroy cancer cells. It is most often used after surgery to the breast and lymph glands but may occasionally be used before surgery. There are lots of different chemotherapy treatments and suitable ones will be explained and discussed with you. It is possible you will be asked to consider entering a clinical trial.
Chemotherapy is given as a course of treatment usually as a day patient or lasting a few days, followed by a rest period of a few weeks. The number of courses you have will depend on the type of cancer you have.
If your chemo is at your local hospital, i.e., South Tyneside or Sunderland, this will be organised by the Chemotherapy Unit there.
The doctor and chemotherapy nurse will be able to explain any side effects to you.
You will be given more information about chemotherapy from the Chemotherapy Unit. If you require any additional information ask your breast care nurse or contact Breast Cancer Care – Freephone 0808 800 6000.
A side effect of chemotherapy is hair loss. If this occurs you will be provided with a wig, free of charge, if you require one. The chemotherapy nurses will advise you how to go about obtaining your wig.
The Queen Elizabeth Hospital also provide a headdress service for those patients who prefer to wear alternative types of head wear such as hats, scarves etc. Trained volunteers will demonstrate the use of those and an appointment can be arranged via the chemotherapy day unit on 445 2575. Appointments usually take 45 minutes.
Herceptin
Herceptin can be given to some patients diagnosed with breast cancer. Not everyone is suitable to have Herceptin, however, all patients who are eligible to have this treatment will receive it.
Herceptin is a drug that treats breast cancer and improves the way the body fights breast cancer cells. Herceptin works by stopping one of the ways that cancer cells divide and grow. Only patients whose cancer has high levels of the HER 32 protein will benefit from Herceptin. This is known as HER 2 Positive breast cancer, and it is found in 20 – 25% of breast cancer patients. Your oncologist will discuss Herceptin with you if this is advised.
Bisphosphonates
Bisphosphonates are a group of medications that are used to treat thin bones (osteoporosis).
Bisphosphonates: why are these drugs used to treat Breast Cancer?
Clinical trials have found that bisphosphonates slightly reduce the risk of breast cancer coming back in patients’ bones and often meant that patients lived longer. Not all patients had the same degree of benefit though.
How do I take Bisphosphonates?
Bisphosphonates can be administered through a drip into a vein or as a tablet using a drug called Zoledronic acid. We recommend you take the treatment over three years. Treatments are given once every six months therefore a total of six treatments are recommended.
If you are already taking an oral Bisphosphonate tablet such as Alendronate, Risedronate or Ibandronate for osteoporosis please discuss this with your oncology consultant or breast care nurse.
Prescription charges
Prescription charges are exempt if you are:
- Undergoing treatment for cancer,
- Experiencing the effects of cancer,
- Experiencing the effects of treatment for cancer
What do I need to do?
You should ask your GP for an application form, called Form FP92A, which they should have a supply of. You will need to make sure that this form is the most recent version, it should have a date no earlier than 1st January 2009 printed on it. Once the form is completed it will then need to be sent to the address on the form. Ask your doctor if you can send it yourself as this is likely to speed the process up.
You will then be sent an exemption certificate which you will need to show the chemist whenever you get a prescription dispensed.
How long does it take to get the certificate?
Once your application is received your certificate should be issued within 7 – 10 days.
When I’ve got my certificate, how do I use it?
Just show your certificate at the pharmacy (chemist) when you need a prescription and complete the medical exemption statement on the back of the form. You will then not have to pay prescription charges.
How long does the certificate last?
The certificate is valid for 5 years. It entitles you to all your NHS prescriptions free of charge, not just those relating to cancer. After five years the certificate can be renewed and then renewed as many times as necessary as long as you are still undergoing treatment for cancer, experiencing the effects of cancer, or experiencing the effects of treatment for cancer.
If you need to stay on your cancer medication for ten years you can reapply for this exemption.
What if my condition changes?
The certificate does not have to be returned if you are no longer undergoing treatment for cancer, experiencing the effects of cancer, or experiencing the effects of treatment for cancer. So you can still claim exemption to prescription charges until the certificate expires.
What if I have paid for prescriptions recently?
Ask for an NHS receipt (FP57) at the time you pay for the prescription, and a refund claim form. Then once you’ve received your exemption certificate take the FP57 receipts and the refund claim form to the chemist or pharmacy and they will provide a refund. It does not need to be the pharmacy that issued the FP57.
Prescription charges you have paid, and have FP57 receipts for, will be refunded back to the date your exemption certificate takes effect (shown on the certificate).
Over 60 and have cancer, do I need a certificate?
People over 60 are already exempt from prescription charges and do not need to apply for a certificate.
If I have already paid for a pre-payment certificate – how do I get a refund?
Depending on how long your pre-payment certificate has left to run you may be entitled to a refund. On the back of your pre-payment certificate is an address to return it once you have received your exemption certificate. You need to send a covering letter with it, explaining that you are now medically exempt from paying for prescriptions and that you would like to claim a refund. Claims for refunds need to be submitted within three months of becoming medically exempt from prescription charges.
Need more information?
- Contact your local Macmillan Cancer Information and Support Service – 0191 445 2979.
- Ring Help with Help Costs helpline on 0845 850 1166.
- Macmillan Cancer Support 0808 808 000 of visit www.macmillan.org.uk
Family History
Most cases of breast cancer seem to arise by chance. Approximately only 5–10% are inherited. Your breast care nurse or surgeon will be able to discuss the risks with you.
As breast cancer in men is uncommon you may be offered a referral to genetics. If relatives are concerned that they are at risk, they should ask their GP to refer them to a breast specialist.
Clinical trials
To enable us to offer our patients the best possible treatment, it is important to us that the Breast Unit is involved in research which will provide answers to important questions. Clinical trials are a way of finding out which treatments are the best.
You will always be offered the best possible treatment that we have, but you may be asked to consider entering a clinical trial comparing that treatment with another which we know is at least as good but may be better. If asked to join a clinical trial everything about the trial will be explained to you and you will be given written information and the opportunity to talk to and ask questions of the doctor, breast care nurse and the research nurse.
The decision to help in a clinical trial is always up to you. You will be given as much time and information as you will need to make up your mind. Even after agreeing to take part in a trial, you can still withdraw at any stage if you change your mind. Your decision will in no way affect the care that you receive. If you choose not to take part or you withdraw from a trial you will receive the best standard treatment rather than the new one with which it is being compared. Whatever you decide you can be sure that we will make every effort to involve you in the planning of your treatment and we will always listen to your views and take these into account.
Follow up care
You will attend outpatients for check-ups. The length of time you will attend for follow up will vary.
Your breasts will be examined on these visits by your consultant, oncologist, junior doctor or your breast care nurse. Mammograms will be organised yearly from the clinic. Please discuss any worries or concerns you have when you attend the clinic with your consultant, oncologist or breast care nurse.
If you have any concerns, worries or new symptoms between your appointments please contact your consultant’s secretary or your breast care nurse for an earlier appointment.
After five years you will need to see your GP as you will be discharged from our care.
If you have any problems with moving your shoulder, ask your doctor, breast care nurse or GP to refer you to the physiotherapist.
Once you have completed your surgery/treatment, your breast care nurse will no longer automatically contact you. If you require any further support, information or advice please do not hesitate to contact your breast care nurse.
Breast awareness
Breast awareness is a part of general body awareness. It is a process of getting to know your own breasts and becoming familiar with their appearance. Learning how your breasts feel at different times will help you to know what is normal for you. You can become familiar with your breast tissue by looking and feeling – in any way that is best for you (e.g. in the bath, shower or when dressing).
Look for changes that are unusual for you, such as a lump or thickening, pain, discharge from the nipple, unusual appearance or sensation. If you find a change that is unusual for you, contact your GP as soon as you can. There may be reasons for changes in the breast. Most of them are harmless but all of them should be checked as there is a small chance they could be the first sign of cancer.
Macmillan service
What is a Macmillan Nurse?
Macmillan Nurses work as part of the team of doctors, nurses and other professionals looking after you.
They give supportive care and advice to patients with cancer.
The care is available from the moment that someone is diagnosed, throughout the course of their lives.
The Macmillan Nurse can be contacted via your GP, District Nurse, hospital doctor or the nurse looking after you.
Financial help
If you have financial problems due to your breast cancer diagnosis, you may be entitled to a Macmillan grant or assistance with travel expenses. Please discuss with your breast care nurse.
Car Parking: You may be entitled to free car parking if you are attending clinics very frequently. Please discuss this with your breast care nurse/Chemo Unit.
Bus Fares: If you are on benefits you can claim your bus fares back by attending the General Office and producing proof of tickets. If you need advice regarding benefits the Macmillan benefits advisor may be able to help. Contact the Cancer Information Centre at Queen Elizabeth Hospital on 0191 445 2979. There is also an advisor at Cancer Connections, South Tyneside, Tel. No. 0191 456 5081.
Cancer Information Centre
If you need further information on any aspect of care, treatment or what is available, please drop in to the Cancer Information and Support Centre (Swan Centre).
The centre is located near the Breast Unit along the medical corridor. No appointment is necessary and the atmosphere is relaxed and friendly. There is a wide variety of information freely available and guided internet access. The centre is open Monday to Friday (except bank holidays) between 10am and 4pm.
The centre offers:
- Information on living with all types of cancer and treatments
- Help with claiming benefits, grants, finding holiday insurance and other financial guidance
There is a large library of materials in different formats and languages, and these are provided free of charge. If you do not wish to come in person, family members or friends are welcome. You may also contact the centre by telephone or letter. Direct Line: (0191) 445 2979
Sunderland Macmillan Cancer Information Centre
The centre is located in Sunderland Royal Hospital, open Monday to Friday (except bank holidays) 10:00am and 4:00pm. Tel: (0191) 454 0122
Maggie’s Newcastle – Located at Freeman Hospital
Tel: (0191) 233 6600
Complementary therapies
A range of complementary therapies are available through Coping with Cancer North East. Contact: 0191 250 2026 and Cancer Connections: 0191 456 5081.
Auricular (ear) acupuncture
Some patients experience hot flushes or other symptoms such as anxiety as a result of treatment for breast cancer. Coping with Cancer provide a service at various locations. If you are interested in finding out more about this service please phone Coping with Cancer on (0191) 250 2026. Your breast care nurse will be able to provide you with further information.
Look good feel better (for men)
Thanks to the support of leading cosmetic companies, a free programme of workshops is held at the Freeman Hospital for patients who are undergoing cancer treatments.
These skin care and grooming workshops help to combat the visible effects of cancer treatments, which in turn, can increase confidence and wellbeing. These sessions are available in person and online.
Anyone wishing to book a place in the Maggie’s Centre, Melville Grove, NE7 7NU, should telephone the Freeman Hospital on 0191 233 6600.
Look Good Feel Better is running sessions at Sunderland Hospital. You are advised to contact Macmillan Cancer Support on Tel: 0191 541 0122 at Sunderland to book sessions. These are held on the first Monday on the month (except Bank Holidays) in the Education Centre. They usually see 10 patients at a time and there is a waiting list. Patients will be invited by letter to attend when it is their turn.
Cancer Treatment and fertility
Having a diagnosis of cancer may make you think strongly about your fertility. This may be something that has always been important to you. However, this may also be something that you need to think about sooner than you had planned.
For some people the possibility of losing their fertility is every bit as difficult as being diagnosed with cancer, for others cancer and its treatment is their only concern. There is no right or wrong way to feel.
Your cancer may be treated by surgery, chemotherapy, hormonal therapy or radiotherapy. All of these treatments can affect fertility in some way, depending on where you have cancer or where the treatment is directed. It can also be difficult to predict how your fertility will be affected.
It is very important you try and avoid getting your partner pregnant while you are receiving treatment for cancer and for up to a year after treatment finishes. You should therefore use a reliable form of contraceptive during this time. A barrier method such as a condom should be used during chemotherapy treatment, whether you are avoiding pregnancy or not, as chemotherapy may be excreted in bodily fluids in small amounts. If you are receiving chemotherapy, you should be provided with more detailed information on sex, relationships and fertility before your treatment starts. If pregnancy occurs during treatment please inform your specialist nurse, GP or cancer specialist doctor as soon as possible as there could be a risk to your unborn child.
Your future
There are several issues to consider when planning for your future:
- preserving your fertility through sperm collection
- embryo storage
- using donated eggs or sperm
These options are not available to everyone for a number of reasons. This may include the need to start cancer treatment immediately.
Further information and support
Cancer treatment and fertility is a very important and complicated issue for many people facing it. The purpose of this information is to highlight this at the earliest opportunity. We have detailed information on both men and women in the Macmillan Cancer Information and Support Centre. You may request this by telephone, via your doctor or Specialist Nurse or by dropping in.
Support services available
There are a number of support services available to you. Here is a list of some of the services available.
Breast Cancer Survival Trust
Macmillan Cancer Relief
Can provide Macmillan nurses, advice and counselling
Cancer Connections
South Tyneside
Provides support, information and complementary therapies
Citizens Advice Bureau
Offers free confidential advice and information including financial
Breast Cancer UK
Breast Cancer now
Offers practical advice and information
General hospital information
Public Transport
A booklet has been designed to give detailed information on all public transport services that visit the hospital. This booklet is available from a wall rack situated within the main entrance to the hospital.
Parking
The hospital operates number plate recognition system, please see the map. Pay machines are located inside the hospital and at the car parks. Disabled parking areas are situated throughout the hospital and there is also provision for cycle and motorcycle parking as well. Although every effort is made to provide secure parking facilities, please ensure that you take care of your property and do not leave anything valuable on car seats where they are visible.
Please contact the Macmillan Cancer Information and Support Centre as soon as possible for further details on applying for a hospital parking pass.
No Smoking Policy
Gateshead Health NHS Foundation Trust operates a strict No Smoking policy and this means that smoking is not allowed in any part of the hospital.
Restaurants and Cafeteria
The main restaurant in the Queen Elizabeth Hospital is called The Hub. This is located on the corridor nearest to the old main entrance, opposite the chapel. It serves a variety of hot and cold drinks, snacks and meals throughout the day.
A tea bar is situated in main outpatients. It is open from Monday to Friday, from 10am to 1:30pm. There are other outlets to buy tea/coffee/food at the new entrance to the hospital.
Hospital Shops
There are several shops situated in the main entrance. They sell a variety of products, including newspapers, drinks, confectionary, food, toiletries, etc. They are open long hours, seven days a week and are usually open from 8am to 8pm.
A cash machine is situated in the newsagents and this takes most bank cash cards. There is a charge for withdrawing money using this service.
Payphones/Post boxes
There are free phones throughout the hospital that will allow you to call a taxi. There is a Royal Mail post box situated outside the hospital shop.
Use of interpreters and other information methods
We can provide interpreters for patients whose first language is not English as well as interpreters in British Sign Language. Patients who require an interpreter will normally be identified by a member of staff when they first attend the hospital, clinic or GP practice. Usually, an interpreter is booked at this time. We discourage patients from using friends and family members as interpreters, unless at the patient’s request. If you have a problem or concern with interpreting please contact the Patient Advice and Liaison Service (PALS) within the hospital.
For patients and visitors whose first language is not English, an interpreter can be arranged.
Verbal information in any language about any cancer is also available by contacting Cancer backup on Freephone 0808 800 1234.
Information materials in other languages are also available through the Macmillan Cancer Information and Support Centre.