This leaflet aims to help you understand and gain the maximum benefit from your operation. It is intended for patients who are either thinking about or have decided to have surgery after discussing this with their consultant or surgical team. Each person’s operation is individual, and you may be given specific instructions that are not contained in this leaflet.
What is shoulder Instability?
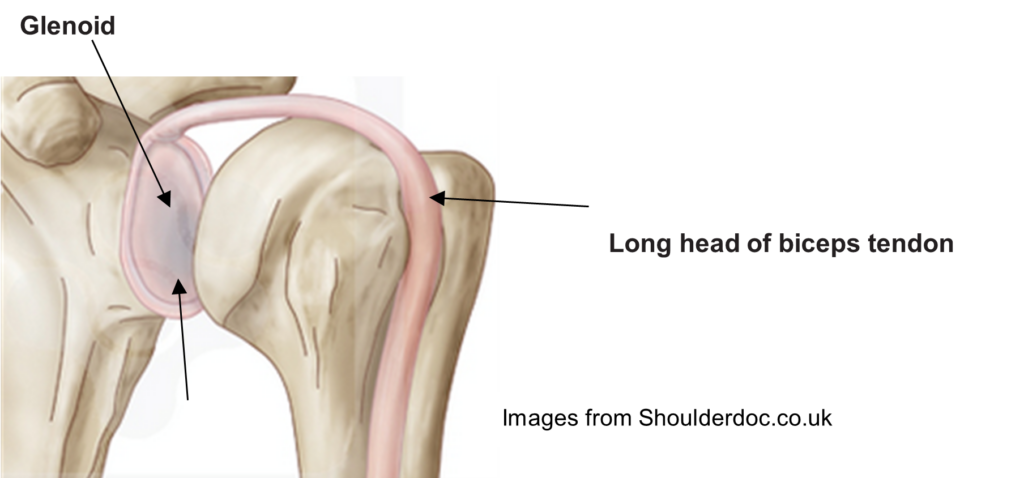
Your shoulder is the most mobile joint in the body due to the configuration of the ball and socket joint. The socket (glenoid) is very shallow which allows it to be increasingly mobile. To compensate for this, it contains a thick rim of tissue (labrum) which surrounds and helps to deepen the socket. Along with the rotator cuff muscles (the main shoulder stabilisers), ligaments (including the joint capsule) and the glenoid labrum (which acts like a bumper to the front and back of the socket), they all assist in keeping the shoulder stable through its normal range of movement.
Shoulder instability can feel like the ball is slipping, catching or coming out of joint. It may be associated with pain and a sense of a ‘dead arm’ and apprehension to move the arm in certain positions. Shoulder instability ranges from the joint feeling like it is slipping (subluxation) to a partial or complete dissociation of the ball and socket joint (dislocation). Shoulder dislocations usually occur at the front (anterior), with a small portion (less than 10%) occurring at the back (posterior).
Dislocations are more common in younger patients and are often a result of an injury or trauma (such as when playing contact sports). For some younger patients, the shoulder is not involved in an injury as such but dislocates due to underlying joint and soft tissue laxity and instability.
During a shoulder dislocation, the structures surrounding the joint including the ligaments and labrum are often injured. This may lead to symptoms of repeated dislocations or the feeling that the shoulder is unstable. Labrum injuries commonly seen with a shoulder dislocation are called a ‘bankart lesion’ and this occurs at the lower part of the labrum. Injuries to the shoulder socket are called a ‘bony bankart lesion’ and this occurs when some of the glenoid bone is broken off with the anteroinferior labrum.
What are the symptoms of shoulder instability?
- Repeated dislocations or subluxations
- Apprehension
- Pain
- Decreased range of movement
What are the treatment options?
- Conservative management – in many cases the combination of physiotherapy, painkillers, activity modification may treat the symptoms of shoulder instability. For those patients that have shoulder instability, which is not associated with any injury or trauma, surgery is usually not indicated.
- Surgery – This may be considered in patients where conservative measures have failed. The aim of surgery is to restore shoulder function, stability and to improve pain. While it is often perceived as a quick and easy fix, in reality, there is a long period of postoperative physiotherapy rehabilitation, and certain risks are associated with the procedure.
Shoulder stabilisation surgery
Depending on the type of surgery it can be performed either as a keyhole procedure (arthroscopic) this involves making 2 to 5 small scars around the shoulder or as an open surgery done by making an open incision that will leave a scar approximately 7cm long at the front of your shoulder.
The aim of shoulder surgery is to repair the torn labrum/ligaments. There are two main types of stabilisation surgery (below), and a member of the surgical team will discuss the type of surgery you may require.
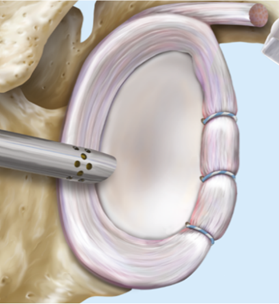
Bankart or labral repair:
This is a soft tissue repair that involves reattachment of the torn shoulder labrum and ligaments.
The surgery is done as a day case arthroscopic procedure. It is rarely done as an open operation.
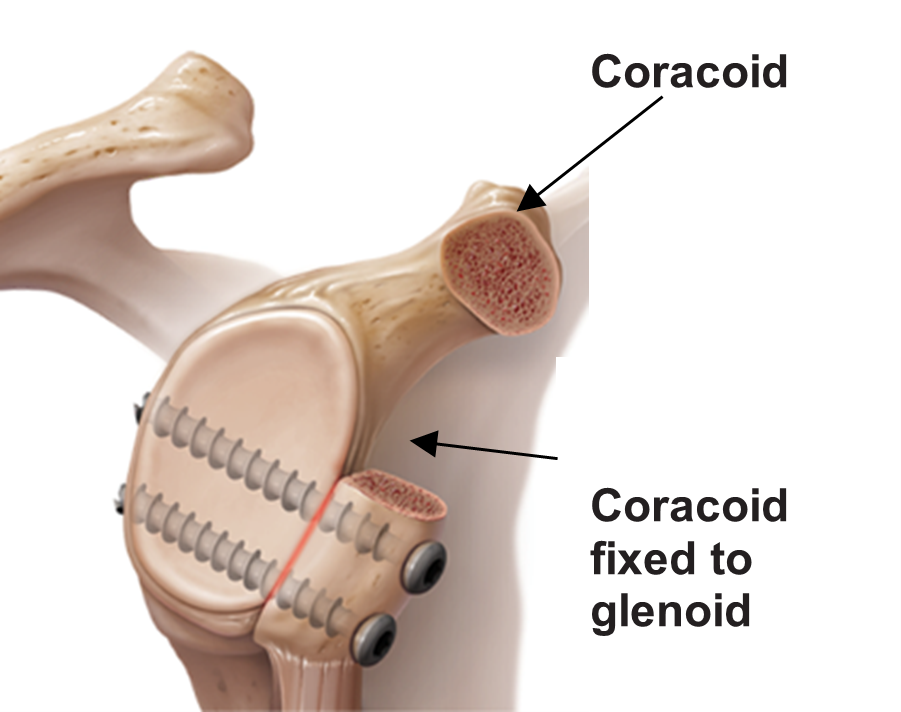
Latarjet procedure:
This is performed when there has been an injury to the bone at the front of the glenoid (socket) or for failed soft tissue repair.
The procedure involves a transfer of the coracoid with its attached muscle to the front of the socket to re-build where the bone has been damaged. This then acts as a support to prevent future anterior dislocations. This is done as an open procedure and the risks of infection, nerve injury and stiffness are higher than in arthroscopic surgery.
Are there any complications with surgery?
All surgical procedures are associated with a degree of risk. The main complications are:
General complications:
- Pain – levels felt after surgery vary for each individual depending upon pain thresholds, the nature of the problem and various other factors. It is not common to have symptoms through the night.
- Bleeding (<1%) during or after surgery.
- Infection of the wound (<1%). After your operation you should contact the surgeon if you get a temperature, notice discharge from your wound, feel unwell, or if your wound becomes red, sore or painful.
- Scar – these usually become invisible over time.
- Deep Vein Thrombosis (DVT) or Pulmonary Embolism (PE) these are uncommon.
- Anaesthetic complications which the anaesthetist will discuss this with you.
Specific complications:
- Persistent pain and or stiffness in the shoulder – It is possible some level of pain remains in the shoulder after surgery. Shoulder stiffness can also occur, and you may not regain full movement in the long term. This should you not limit your ability to use your shoulder.
- Nerve or blood vessel injury is very rare (< 1%). Numbness and paraesthesia (tingling) are the usual symptoms. Most nerve injuries usually resolve in time, however permanent nerve damage may occur.
- Recurrent instability or re-dislocation (<10%) sometimes the repair can fail and result in further instability of the shoulder. This may require revision surgery.
- Revision (repeat) surgery – the results are generally less favourable compared to primary surgery. Similarly, complication rates and risks are usually higher in revision surgery.
What happens before the operation?
Pre-admission assessment
This is an assessment of your health to make sure you are fully prepared for your admission, treatment and discharge. Please bring a list of all your current medication including a list of allergies and the type of reactions. Before the date of your admission please, read very closely, the instructions given to you by the pre-admission assessment and your confirmation appointment letter.
Planning ahead
Once you have your date for surgery you can do several things to aid preparation for your operation and to improve your recovery. It is important to plan and make arrangements for how you will manage when home. Stocking up your freezer with easy cook items is advised (particularly if you live alone), as you may find daily tasks such as cooking more difficult initially after your operation. If you have family or friends who can stay with you or visit regularly this may make your recovery easier both for helping with household tasks and moral support.
Smoking
Smoking has been shown to delay wound healing and increase complications after surgery. Patients who stop smoking benefit from long term improvements to general health, decrease the risks associated with anaesthetic and have a better outcome from surgery. If you are interested in stopping smoking, please speak to your pre assessment nurse or GP for advice and services available.
Cancellation
If you are unable to attend your appointment, please contact us immediately so that we can offer your appointment to another patient.
Anaesthetic
Shoulder stabilisation surgeries are usually performed under a regional anaesthetic (nerve block) with or without a general anaesthetic (which puts you to sleep). A regional anaesthetic will numb the affected arm and will assist with pain control after the operation. It can take up to 24 hours before this completely wears off, during this time, you will not be able to move your arm and you may have some altered sensation of the arm or hand that persists for some weeks. The anaesthetist will see you before your operation and discuss your anaesthetic with you.
Day of surgery
You will be given specific instructions about when to stop eating and drinking, please follow these carefully as otherwise this may pose an anaesthetic risk and we may have to cancel your surgery. You should bath or shower before coming into hospital.
The anaesthetist, surgeon or a member of the team will visit you and answer any questions you may have. You will be asked to sign a consent form. A cuff will be put on your arm, some leads placed on your chest, and a clip attached to your finger. This will allow the anaesthetist to check your heart rate, blood pressure and oxygen levels during the operation. You might just receive an injection into the side of your neck (nerve block) to numb your shoulder; you will remain awake during the procedure. If you have a general anaesthetic, a needle will be put into the back of your hand to administer the drugs to send you to sleep.
Hospital stay
Shoulder stabilisation is usually done as a day case procedure, however depending on your recovery after the operation and your home situation you may be required to stay overnight.
Recovery after surgery
The following leaflet gives you advice as to when you may be able to do things, however your progression depends on the type of surgery, and you should always be guided by your physiotherapist/surgeon.
After surgery you will see a physiotherapist in the recovery room. They will give you advice regarding using your sling and also the appropriate exercises. You will be referred to physiotherapy for ongoing rehabilitation and an appointment will be made for you.
When do the stitches come out?
The stitches will be removed either in an orthopaedic clinic or at your GP surgery, usually 10-14 days after your operation. Keep the wound dry until it is fully healed.
If you get a temperature, become unwell, if your wound becomes red, sore and painful or you notice pus, always contact the ward or your consultant’s secretary immediately.
Pain
You will be given appropriate painkillers on discharge from hospital. If you feel you are unable to manage your pain, please discuss this with your GP, surgeon, or physiotherapist.
Wearing a sling
On return from theatre your shoulder will be in a sling to protect the shoulder during the healing period. You will be advised how long to wear a sling for by your physiotherapist/surgical team. You must not remove your sling except for washing, dressing and appropriate exercise. Ensure that your wrist and hand is correctly in the sling.

Sleeping
Your sling must be worn in bed. We would recommend that you lie on your back or on the opposite side. You should not lie on your operated shoulder for the first 6 weeks. If you are lying on your back to sleep, placing a pillow under your upper arm/elbow can make it more comfortable.
When lying on your non-operated side, you can fold or hug a pillow in front of you to support the arm. You can also tuck a pillow along your back to help prevent rolling onto the operated shoulder. It may also be comfortable to sleep in these positions once the sling has been removed.


Washing and dressing
When washing or dressing you may find it more comfortable to support your arm on a pillow while it is out of the sling. Wearing loose clothing with front fastenings maybe easier after surgery. When getting dressed, dress your operated arm first and when getting undressed, this arm comes out last.
Daily Activities
Although your shoulder stability surgery has been completed it takes time to heal. You will need to use your non-operated arm for activities like eating, dressing, and cooking for the first 3-6 weeks. You will need to protect the operated arm and avoid heavy lifting or strenuous exercise. It is normal for you to feel discomfort, aching and stretching sensations when you start to use your arm. Intense and lasting pain (e.g., for 30 minutes) means that you should reduce that activity or exercise.
Physiotherapy/Exercises
You will see a physiotherapist on the day of surgery. They will give you advice on how to wear the sling and provide you with specific exercises to start moving your arm safely once the block has worn off. It is important to move your shoulder to prevent it from becoming stiff but do not stretch or force it initially to protect the repair. The exercises may feel uncomfortable or give you a pulling sensation, but they should not cause pain. You will gradually be able to start using your arm for light activities.
Once you have regained good movement and control of your shoulder the physiotherapist will work with you to build upon your strength and endurance. Your individual rehabilitation goals will be discussed with you regarding returning to a particular activity or sport. We do advise that returning to contact sports is discussed with your consultant or team prior to returning. It may take 6-9 months before you can return to play depending upon your surgery. Within 6-9 months you should regain your movement and strength although further functional recovery may take up to 1 year.
You will be referred to physiotherapy after your surgery. If you have not received a physiotherapy appointment within 2 weeks of your operation, please contact the physiotherapy team on the number(s) below.
Physiotherapy locations
Please note, depending on the location of your GP, the physiotherapy provider may be different:
- If you have a Gateshead / Newcastle GP, your physiotherapy provider will be Tyneside Integrated Musculoskeletal Service (TIMS). If you have a query about your first appointment with TIMS, please contact the booking team on 0191 445 2643
- If you have a Durham GP, your physiotherapy care will come under Durham. Please contact the Queen Elizabeth hospital, physiotherapy department should you not receive your first appointment on 0191 445 2320
- If you have a GP that is outside of the Gateshead / Newcastle or Durham area and you have had elective surgery, your physiotherapy will be at the Queen Elizabeth hospital. If your surgery is due to trauma, your physiotherapy provider will be with the hospital affiliated to your GP practice. Should you not receive your first appointment, please contact physiotherapy reception on 0191 445 2320
Driving
We advise that you do not drive for at least 6-8 weeks after your operation. This is to protect the surgical repair. It is wise to discuss this with your insurance company before you return to driving.
Work
You may be off work between 4-12 weeks following surgery. This is dependent on the type of work you do, the arm which has been operated on and if you need to drive. It is advised not to perform any heavy lifting, overhead or manual work for 4-6 months after surgery. Please discuss with the surgical team.
Flying
Discuss with your consultant and with the airline’s medical department if you wish to fly within 6 weeks of your operation due to the risk of clot formation.
Your recovery
The recovery time after shoulder stabilisation surgery is variable for everyone. However, after 6 months there will be a significant improvement and after the full 9 months rehabilitation period, we would hope to see a significant reduction in pain and a good level of function. If you had open surgery, your estimated progress will be slightly slower.
Functional activities (these are minimum times and could be longer)
Depending upon your surgery, recovery, movement and strength in your shoulder, the timelines below may differ. Please use this as guidance and discuss with your surgical team prior to participating in activities.
| Swimming | Breaststroke Front crawl | 6 – 8 weeks 12 – 16 weeks |
| Cycling (non-competitive) | Road | 8 – 12 weeks |
| Racquet sports | Operated arm | 12 – 16 weeks |
| Specific sport | be guided by your physiotherapist /surgeon – there is no guarantee you will be able to return to your pre injury level of activity |
Telephone numbers
| During the hours of 8am – 8pm contact the Day Surgery Unit, Peter Smith Surgery Centre, Queen Elizabeth Hospital | 0191 445 3009 |
| During the hours of 8pm – 8am contact Level 3, Peter Smith Surgery Centre, Queen Elizabeth Hospital | 0191 445 2028 |
| During the hours of 08:00 – 16:30 contact the Physiotherapy Department | 0191 445 2320 |
| During the hours of 8am – 8pm. If you have a Gateshead or Newcastle GP, TIMS will be your physiotherapy provider If you have a query about your first appointment with TIMS please contact our booking team on 0191 445 2643 If you are a current TIMS patient and have a query about your follow-up appointment, please contact our local admin team on 0191 213 8800 | Booking Team: 0191 445 2643 Local Admin Team: 0191 213 8800 https://www.tims.nhs.uk/ |
| Main Switchboard | 0191 482 0000 |