Radical Trachelectomy
This information leaflet provides specific information about your surgery and should be read alongside the ‘Gynaeoncology patient information to prepare for your surgery and recovery’
What is a Radical Trachelectomy?
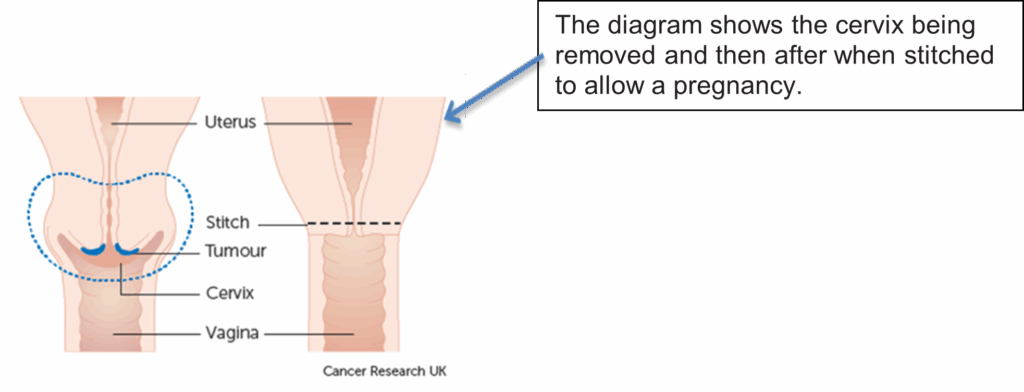
A trachelectomy is an operation for early-stage cervical cancer that preserves fertility for women who still wish to have children. The procedure involves the removal of the cervix (neck of the womb), tissue around the cervix (parametrial tissue) and a small section of the upper part of the vagina. The uterus (womb) ovaries and tubes are left in place. A sample of pelvic lymph nodes are taken because the cancer can spread to these nodes. These nodes will be tested to see if they contain any cancer cells.
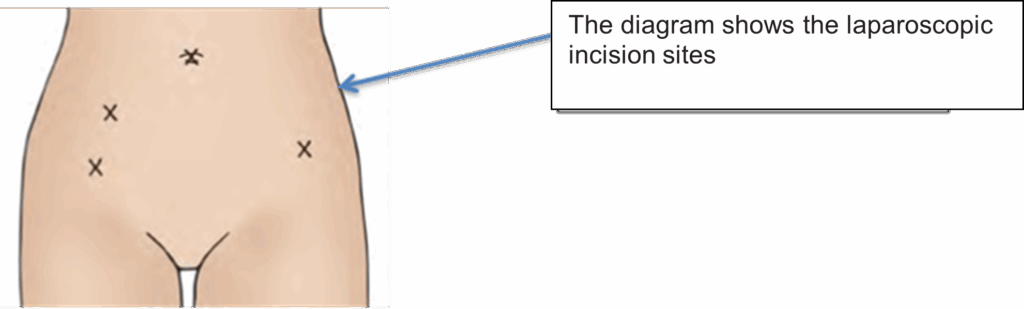
This surgery may be performed vaginally with keyhole surgery or through a cut in your tummy. Your surgeon will explain which approach will be needed for you and why. A large permanent stitch is inserted around the opening to the uterus (womb) which is strong enough to support a future pregnancy but still allows you to have your monthly period and to conceive. Babies have to be born by caesarean section after this operation.
Can there be any complications or risks associated with this surgery?
- General anaesthetic carries a small chance of complication. This will be discussed with your anaesthetic doctor before your surgery. It is important to realise that these risks and complications are rare, and every care is taken to keep the risks as low as possible.
- Infection- The risk of post-operative infections is reduced by giving preventative antibiotics around the time of surgery, but infection can still sometimes occur in the chest, wound, pelvis or urine. Infections are usually easily treated with antibiotics.
- Bleeding (hemorrhage) – This may occur during the surgery or rarely afterwards. Blood transfusion is required in around one in five surgeries. You may need to return to theatre in the rare case of internal bleeding after the surgery.
- Clots (thrombosis) – It is possible for clots of bloods to form in the deep veins of the legs and pelvis. This is called a deep vein thrombosis (DVT). This will normally cause pain and swelling in the affected leg and is relatively simply to treat using blood thinning drugs. In rare cases it is possible for a clot to break away and be deposited in the heart or lungs. If this occurs it is a potentially serious complication, but several measures will be taken to reduce the risk of this happening. Moving around as soon as possible after your surgery can help as can wearing special surgical stockings and having injections to thin your blood. With every surgery there is a very small risk of death.
Risks specific to this type of surgery include:
- Lymphoedema – may occur when the lymphatic drainage system becomes blocked and surrounding tissues may swell, causing swelling in the lower body and legs. This can lead to skin problems, pain and discomfort. This can become permanent and can happen months or even years after surgery. Some early research suggests that this will affect less than five in 100 of patients having this procedure.
- Lymphocyst or lymphoceles – these are swellings filled with fluid that develop in your abdomen after your operation. They are often naturally re-absorbed by your body, but if they are larger or causing you discomfort, your surgeon may drain them by using local anaesthetic and a needle.
- Bladder problems – a small number of women will have difficulty emptying their bladder after this surgery and may need to go home with a catheter in their bladder for several weeks. A very small number of women may have long-term difficulties with emptying their bladder, but this is rare.
- Problems with menstruation (your periods) – some women may find that the blood from their menstrual cycle (monthly period) becomes trapped inside the womb as the entrance is too small for it to drain away fully. If this happens, you will need to have a minor surgical procedure to open the entrance to the womb. A small tube called a ‘Smitt sleeve’ or a ‘coil’ can be inserted into the opening to the womb to keep the entrance open.
- Late miscarriage/preterm delivery – There is a risk of late miscarriage or preterm delivery when you have had a trachelectomy. Please discuss this with your gynae- oncology team.
- Delivery by caesarean section – if you are pregnant following your radical trachelectomy, we will refer you to a high-risk obstetrician as your baby will need to be delivered by caesarean section. Please speak to your surgeon or clinical nurse specialist if you have further queries.
What are the alternatives to having this surgery?
The other surgical intervention that you could get is called a radical hysterectomy. A radical hysterectomy is where the womb is also removed alongside the cervix, the tissues surrounding the cervix and the top part of the vagina. With a radical hysterectomy this would prevent you carrying any future pregnancies. If your ovaries are retained, it could be an option to use your eggs for a surrogate mother. If you wish to discuss fertility options further, we will refer yourself to the specialist team based at the Centre for Life in Newcastle to discuss all options with you.
What additional help/support around fertility will I get?
If you are considering getting pregnant following this surgery, we will refer you to the Centre for Life in Newcastle with the fertility team to discuss what options you have. Also, a referral will be made to a high-risk obstetrician so they can discuss any questions/concerns around pregnancy.
Should I continue to have cervical smears?
Yes. The cervix has been partially removed and therefore annual smears are still recommended.
Giving your consent for surgery
Before you have an operation, you must sign a form to give consent (permission) for the doctors to treat you. The doctors may ask you to sign the form in clinic, at your pre-assessment appointment or when you are admitted to hospital. Your surgeon will discuss with you in more detail your individual risks, it is very important that you understand these risks and have all your questions answered before you sign your consent form.