This leaflet has been produced to give you general information about a proximal humerus fracture. It will provide advice and guidance as to what to expect following the injury and exercises to help. If you require further guidance, please do not hesitate to contact your physiotherapist.
What is it?
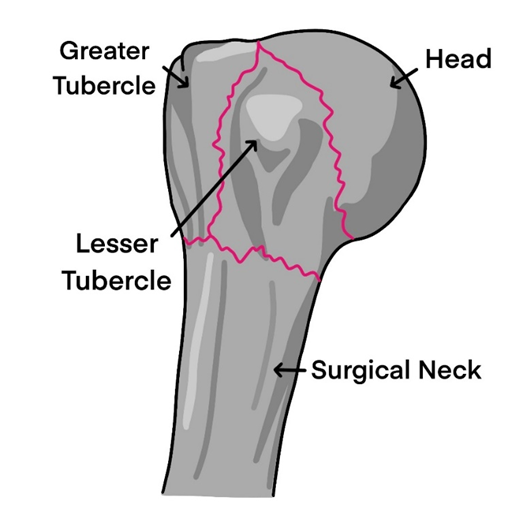
Your shoulder is a very mobile joint made up of your shoulder blade (scapula) and upper arm bone (humerus). A proximal humerus fracture occurs at the upper part of your humerus bone.
Why did it happen?
This type of fracture or break is often caused by falling on to your arm and can occur in any age group but is more common in adults over the age of 65.
Signs and symptoms:
- Pain
- Swelling
- Bruising
- Decreased movement of your shoulder
What should I expect?
You will be reviewed in fracture clinic, or your x-ray will be reviewed by a doctor in a virtual clinic soon after your injury and then again between 2-4 weeks later. If your bone is healing well, you may be discharged from the doctor, but your physiotherapy will continue for some time after.
The arm can be very painful especially in the first few weeks. It is common to experience bruising, stiffness of your shoulder and sometimes this can extend in to the elbow and hand. The main aim of treatment is to prevent stiffness, reduce pain and restore function. It can take 6 to 12 weeks for your fracture to heal, however your symptoms will likely continue for some time after.
It is important to work hard with your exercises for several months after your injury. Improvement should continue for 12 – 18 months; with most people regaining a functional range of movement to perform day to day activities but you may not achieve full range of movement.
How will it be treated?
Most proximal humerus fractures do not need surgery but this depends on the type of injury. In some instances, surgery is required to fix the fracture or replace the joint. Your doctor will discuss this with you.
Sling
Most fractures involve a short period of immobilisation, usually wearing a collar and cuff for comfort. This is usually worn for 3 – 6 weeks depending on your fracture, you will be advised when you can start to wean from this. Your physiotherapist / orthopaedic team will guide you.
Exercises
Early shoulder mobilisation is important to increase your function and prevent long-term stiffness. You may begin this when advised to do so, usually around 2-3 weeks after your fracture. This leaflet, and your physiotherapist / orthopaedic team will guide you. You can start moving the hand, fingers and elbow immediately.
How can I manage my pain?
Regular pain relief is advised. If unsure, discuss with your clinician or pharmacist. It is common to get pain from your shoulder down into your arm.
You may find it more comfortable sleeping in an upright position at first, gradually lying flatter as your pain settles. Place a pillow behind your shoulder and elbow for comfort.
Physiotherapy
After leaving hospital or being seen in fracture clinic, you will be referred to physiotherapy. The physiotherapist will guide your movements and activities and may make changes to your exercise programme depending on your individual needs. It is important to continue regular pain medication to allow gentle movement.
Armpit hygiene
To wash under your arm, take your arm out of the sling and lean forwards slightly so that your arm hangs slightly away from your body. You can also do this in sitting if you have poor balance.
Early rehab
Within the first 2 weeks, recovery is based around comfort and completing hand, wrist and elbow movements to prevent stiffness.
We would encourage you to use the arm for light functional activities at the elbow such as using a knife and fork or doing up buttons of a shirt. Let pain guide you.
As the bone begins to heal, shoulder movements may be progressed and you will be advised when you can start moving by the orthopaedic team. Passive movements play a key role in avoiding shoulder stiffness at this time. It is important to be consistent with your exercises to prevent long-term stiffness and dysfunction.
You may feel some mild discomfort during these exercises but if you feel a significant increase in pain then stop doing that particular exercise until you can seek advice from your physiotherapist.
Repeat these exercises 5- 10 repetitions, 4 – 5 times per day
Early exercises (first 0 – 2 weeks)
Elbow Movement
Bend and straighten your elbow, using the other hand to help if needed.
Elbow Movement
Support your forearm and turn your palms up to face the ceiling and turn them down to face the floor as pain allows.
This movement should occur at your elbow and not your shoulder.
Hand, Wrist and Finger Movement
Move the wrist up and down.
Make a full fist and stretch your fingers out wide.

Later exercises: from 2 – 3 weeks
Again, all exercises must be performed within the limits of tolerable pain. Please do these exercises regularly at home, attempting at least 5 – 10 repetitions, 3 times per day. Do not force or stretch. Continue to take regular painkillers.
Seated Exercise
Sitting down.
Support your painful side with your opposite hand. Slide your hands down your thigh as far as is comfortable, return to the start position.

Pendulum Exercise
Resting your non-injured arm on a table, bend at the waist & let your painful arm hang forward.
Make a circular or forwards and backwards motion with your whole arm.
Don’t do this if you have poor balance.

Table Walk Aways
Rest your hands on the edge of sink or work top. Walk back until you feel discomfort. Nice and gently to start with.
You can wash under your armpit whilst the arm is supported.
Table Top Slides
Sit or stand. Place your hands on a table on a towel or kitchen roll.
Start with the hand of your painful arm on top of your other hand to help it. Slide your hands along the table, reaching forwards and straighten your elbows as much as possible. Slide your hands back. Do small movements to start with.

External rotation with a Stick
Sit or lie down with both elbows bent at right angles.
Place a rolled towel between your elbow and side if sitting down. Hold a stick with both hands.
Gently push the stick to move the hand outwards, keeping your elbow in at your side.

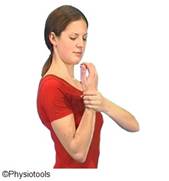
Active Assisted Flexion
Sitting down. Support your painful arm with the opposite hand.
Gently lift the arm as far as it will move comfortably. Do not force.
When you feel comfortable with the above exercises, you may be able to progress on to the following but only do within limits of tolerable pain.
Assisted Shoulder Flexion
Lying on your back, elbow bent. Clasp your hands or hold at your painful arm’s wrist. Straighten your arms towards the ceiling.
If you can, you can take the arm overhead but only if it is comfortable.

Hand Behind Back
Stand tall. Relax your shoulders. Place one hand behind your back and gently slide it along your back to the midline. Gently release to the starting position. Help with your other hand if you can.
Nice and gently to start with. Let pain be your guide with this.

Physiotherapy
You will be referred to out-patient physiotherapy and an appointment will be sent out in the post. The physiotherapist will progress your exercises and assist in your recovery. Continuing the exercises at home will enable you to gain maximum benefit from your operation. This may continue for many months until both you and the physiotherapist are happy with your progress.
If you have not received a physiotherapy appointment within 2 weeks, please contact the physiotherapy team on the number(s) below.
Physiotherapy locations
Please note, depending on the location of your GP, the physiotherapy provider may be different:
- If you have a Gateshead / Newcastle GP, your physiotherapy provider will be Tyneside Integrated Musculoskeletal Service (TIMS). If you have a query about your first appointment with TIMS, please contact the booking team on 0191 445 2643
- If you have a Durham GP, your physiotherapy care will come under Durham. Please contact the Queen Elizabeth hospital, physiotherapy department should you not receive your first appointment on 0191 445 2320
- If you have a GP that is outside of the Gateshead / Newcastle area your physiotherapy will be with the hospital affiliated to your GP practice. Should you not receive your first appointment, please contact physiotherapy reception on 0191 445 2320
TIMS physiotherapy centres
| Royal Victoria Infirmary Queen Victoria Road Newcastle upon Tyne NE1 4LP | Freeman Hospital Freeman Road High Heaton Newcastle upon Tyne NE7 7DN | |
| Bensham Hospital Fontwell Drive Gateshead NE8 4YL | Gateshead Queen Elizabeth Hospital Queen Elizabeth Avenue Gateshead NE9 6SX | Blaydon PCC Shibdon Road Blaydon NE21 5NW |
SMOKING CESSATION
Evidence suggests that smoking can delay fracture healing times. In more extreme cases, it can prevent your fracture from healing at all. Stopping smoking during your recovery will likely aid in the fracture healing process. For more details, please see below.
Useful websites
If you would like further information about health conditions and treatment options, you may wish to have a look at the NHS website at www.nhs.uk or the following https://www.tims.nhs.uk/
For help with smoking cessation visit https://www.nhs.uk/better-health/quit-smoking/?WT.mc_ID=JanQuitSmokingPPC&gclid=EAIaIQobChMI_pL37N7U9QIVF-DtCh0czA0OEAAYASAAEgIwXfD_BwE&gclsrc=aw.ds
Versus arthritis website: https://www.versusarthritis.org/
Telephone numbers
| During the hours of 8am – 5pm contact the orthopaedic department | 0191 445 8500 |
| During the hours of 8am – 4.30pm contact the physiotherapy department | 0191 445 2320 |
| During the hours of 8am – 8pm. If you have a Gateshead or Newcastle GP, TIMS will be your physiotherapy provider. If you have a query about your first appointment with TIMS please contact our booking team on 0191 445 2643 If you are a current TIMS patient and have a query about your follow-up appointment please contact our local admin team on 0191 213 8800 | Booking Team: 0191 445 2643 Local Admin Team: 0191 213 8800 https://www.tims.nhs.uk/ |
| Main Switchboard | 0191 482 0000 |