What is an oesophageal stent?
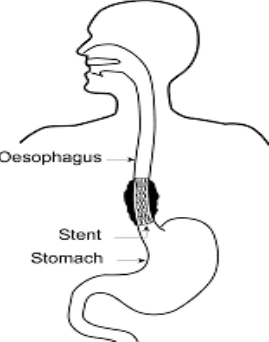
A stent is a tube made of flexible metal mesh which once in position across the narrowed area of your gullet expands to allow fluid and food to pass through to the stomach more easily.
Why do I need an Oesophageal Stent?
The results of a previous Gastroscopy test or barium swallow examination have shown you have a blockage or narrowing in your gullet. Other alternatives would have been considered, but a stent insertion has been proposed as the best treatment option for you.
How is the stent inserted and positioned?
A gastroscopy is carried out using a long flexible instrument called an endoscope. This is about the thickness of your index finger with a bright light at one end. The endoscope is placed into your mouth and guided into your gullet and if necessary your stomach and duodenum. All patientswho are having a stent inserted are given intravenous sedation often in combination with a painkiller. The procedure is will be carried out using x-ray equipment. The abnormal area of the gullet will be identified and its position marked. Having assessed and prepared the abnormal part of the gullet in this way, the endoscope is finally used to position a fine wire into your stomach. The endoscope is then removed leaving the wire behind. The stent is designed so that in its unopened form and can be passed over the wire and carefully positioned.
Once the endoscopist is happy with the positioning, the stent will be released gently to expand and restore the diameter of the gullet and the wire will be withdrawn.
What are the risks?
Stent insertion is generally safe and you can usually go home the same day, but as with most medical treatment, there are some risks. These include:
- Some people get heartburn afterwards. This can be controlled with medicine if necessary.
- Occasionally a stent may slip out of position and the procedure will need repeating.
- Serious complications due to a stent insertion are rare. Serious (life threatening) bleeding is reported to occur in 4 out of every 100 patients who have the procedure, whilst a tear in the oesophagus (perforation) occurs in between 1 to 2 out of every 100 patients who have the procedure. Both of these may require emergency treatment.
- Occasionally, it may not be possible to place a stent despite the doctor’s best efforts. If this is the case the doctor will discuss other treatments with you afterwards.
If you require sedation there is a small risk that the sedative may affect your breathing. We aim to reduce this risk by assessing your general health before the endoscopy and you will be closely monitored by qualifies nurses before and after the examination.
The medications you may receive
Local anaesthetic throat spray
- The spray numbs the back of your throat to make it more comfortable to swallow the tube. You will be fully awake whilst the test is being performed. We will take you to recovery to monitor you for a short while to rest and recover. You can drive yourself home and carry on with your usual activities. You will not be able to eat or drink for 1½ hours after the test, until you can swallow as normal.
Midazolam and Fentanyl
- Midazolam is a sedative injection which aims to make you feel relaxed and fentanyl is a painkiller. They are given through a small needle in your arm or hand once you are in the procedure room before the test begins. Both of these treatments can affect your mental ability to think clearly for up to 24 hours after they are given, even though you may feel wide awake. If you have sedation and painkiller you must have someone to collect you from the endoscopy department and stay with you for the next 24 hours. We will not be able to give you any sedation if you do not have a responsible adult to collect you and stay with you for 24 hours.
Midazolam is a sedative which can affect your mental ability to think clearly for up to 24 hours after it is given, even though you may feel wide awake.
For 24 hours after the procedure you should not do any of the following:
- Drive a vehicle or motorbike
- Use kitchen appliances such as a cooker
- Have a bath unsupervised
- Look after children on your own
- Go to work
- Operate any potentially dangerous machinery
- Sign any legal documents
- Drink any alcohol
- Take sleeping tablets or recreational drugs
- Breastfeed
If you have sedation you must have someone to collect you from the endoscopy department and take you home. You are advised to have someone with you for the next 24 hours, as your judgment will be affected by the sedative. We will not be able to give you sedation if you do not have a responsible adult to collect you and stay with you for 24 hours.
What should I do before my procedure?
Your regular medication should be taken as normal before your test unless you have been advised otherwise by a health care professional.
If you have diabetes you should not take your diabetic medication whilst you are not eating food.
An endoscopy nurse will either see you in preassessment clinic or telephone you before your test, especially if you are taking diabetic medication, warfarin or clopidogrel tablets.
On the day of the procedure
To allow a clear view of your stomach it must be empty:
- Do not have any solid food or milk for 6 hours before your test
- You may have clear fluids only up to 2 hours before your test
- If you are attending for an appointment after 5pm you must not have solid food 10 hours before your test
It is important that you do not starve for longer than this, unless specifically advised by the doctor / nurse, to avoid dehydration.
On arrival in the endoscopy department, please give your name to the receptionist. Your appointment time is the booking in time, not your procedure time. We will try to start your procedure as soon as possible. You may wish to bring a book, newspaper or magazine to read as you wait. Delays can occur, this is mainly due to clinical reasons including emergency situations. We will try to keep you updated with any delays in the unit.
Before the test, you will be seen by a nurse who will go through the health questionnaire with you. A doctor will speak to you in a private area of the department before your procedure. This will give you the opportunity to ask any questions. You will then be asked to sign a consent form indicating you understand the nature and risks of the procedure. You are not required to change out of your usual clothing.
You will be asked whether you prefer a local anaesthetic throat spray or a sedative injection.
What should I expect during the procedure?
The nurse caring for you during the test will ask you to lie on your left-hand side on a trolley. If you have spectacles, hearing aids or dentures you will be asked to remove them for the test. Oxygen will be given to you by a small tube into your nose and a small plastic mouth guard will be placed in your mouth. A nurse will monitor your pulse rate and oxygen levels during the test. During the test air is used to inflate your gullet and stomach to allow a clear view. The air is sucked out at the end of the test; however, you may get “windy” type symptoms and a sore throat. This will usually pass within 24 hours. You may also feel a slight discomfort when the stent is expending within the gullet, this is short lived. If you get a lot of saliva in your mouth, the nurse will clear it using a sucker. The test takes approximately 20-30 minutes.
Does it hurt and will I be in much pain?
The examination may result in some abdominal discomfort due to the stomach being inflated with air. This discomfort should begin to settle once the procedure is finished.
After the procedure
You will either be kept on the endoscopy unit for four hours afterwards or go to a ward to recover fully. This will allow time for the stent to expand.
Approximately four hours after the procedure you will be taken for an x-ray to check the position of the stent and to make sure there are no problems with it. If the stent position is correct you will be allowed to have sips of water. The stent may not fully expand for 3 days and during this time you may experience some chest or back discomfort. This usually settles after a day or two. If you do not experience any difficulties in swallowing you will be allowed to drink fluids only for the following 24 hours. You can try eating very soft (pureed) foods diet the following day, and then onto a soft diet after that.
What kind of food can I eat?
It is advisable to begin by liquidising meals and progressing to soft, moist foods if you feel comfortable. There are some foods that may be difficult to swallow and you should avoid them as they can block your stent. However, general advice is given below:
- Sit upright when you eat or drink
- Take small mouthfuls of food
- Eat slowly and chew your food well
- Use plenty of sauces, gravy and butter to moisten food
- If your appetite is poor, try to have small and frequent nourishing meals
- Try to have warm drinks whilst eating to prevent the tube from blocking
- Keep your teeth and dentures in good order so that chewing is effective
- Clean your stent after eating by drinking soda water or other fizzy drinks.
What to do if you think the stent may be blocked?
There is a small risk that the stent can become blocked, either due to food or because the tumour has grown around the stent. If this happens you will experience increasing difficulty swallowing and food and liquid may be regurgitated (brought back) into your mouth.
You may experience pain on swallowing if you have an oesophageal stent, or pain and swelling of your tummy if you have a gastric stent. If you suspect your stent is blocked stop eating, drink a little water and walk around a bit. This may be enough to clear the blockage if it is due to food.
If symptoms persist contact either the endoscopy unit where the stent was inserted or speak to your nurse specialist at the hospital. If you experience problems outside the normal working day, please contact your GP who will arrange for you to be seen at the hospital. A further endoscopy may be needed to unblock the stent. Depending on how well you are, arrangements may be made to bring you into hospital before this is carried out.
How will I know the results of my test?
The doctor or nurse endoscopist performing the procedure will often be able to give you some results after the procedure. Before you are discharged you will be given clear details concerning any follow up arrangements. A full report will be sent to your referring consultant.
Contact numbers
If you have any further questions, you should contact the following:
Queen Elizabeth Hospital (main switch) 0191 482 0000
Out of hours
Accident and Emergency 0191 445 2171
Endoscopy Unit
Endoscopy department
Queen Elizabeth Hospital
Sherriff Hill
Gateshead
Tyne and Wear
NE9 6SX
If you require ambulance transport please contact your GP Surgery.