What is MASLD?
Fatty liver disease is when you have too much fat in your liver. In a healthy liver there should be very little or no fat. For most people carrying a little bit of fat in your liver will cause you no problems. Too much fat in your liver is as a result of a build-up of fats called triglycerides. They belong to a group of fatty waxy substances which are called lipids. Lipids are used by your body for growth and energy.
We get triglycerides from the food that we eat; foods high in fat and sugar contain high amounts of triglycerides. Triglycerides can also be made in your liver from both sugars and proteins. Your liver processes and controls the release of triglycerides. Triglycerides combine with special proteins resulting in tiny spheres (called lipoproteins) which circulate in your blood stream amongst the cells of your body. When the release of lipoproteins from your liver is interrupted or the flow of triglycerides to your liver has increased there will be a build-up of fat in the cells of your liver.
If you drink too much alcohol this can also cause an accumulation of fat in the liver and can also spur the liver on to make more triglycerides. Fatty liver associated with alcohol consumption is called alcoholic liver disease.
Fatty liver that is not caused by alcohol is known as metabolic dysfunction-associated steatotic liver disease which can lead onto non – alcoholic steatohepatitis.
The first stage of fatty liver disease is steatosis – this is when fat accumulates in the liver without causing any inflammation or scarring. For some the condition will not advance and the development of a serious liver condition will not develop. But for some people MASLD can progress onto non – alcoholic steatohepatitis (NASH). This is a more significant condition, and it could result in scarring to your liver, which can progress to cirrhosis which can cause irreversible damage and is the most severe stage of MASLD.
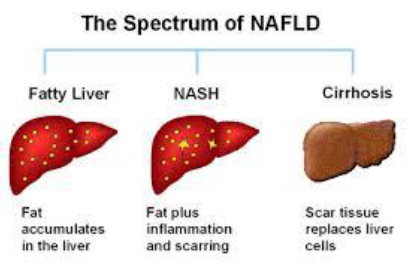
Non – alcoholic steatohepatitis (NASH) is a more aggressive form of MASLD where the inflammation in and around the fatty liver cells could cause swelling and discomfort around your liver. If you place your hand over the lower right side of your ribs it will cover the area where your liver sits. Over a long period of time ongoing inflammation leads to a build – up of scar tissue, this process is known as fibrosis, which can lead onto cirrhosis.
Clinical knowledge about MASLD is still developing but common risk factors are:
- Obesity
- Lack of physical exercise
- Insulin resistance
People most at risk of developing MASLD are those who are:
- Overweight
- Have a poor diet, and do little or no exercise
- Smoke
- Have insulin resistance
- Have type 2 diabetes
- Have high blood pressure
- Have too many triglycerides or cholesterol in their blood
- Have polycystic ovaries
- Have hepatitis B or C
- Are taking certain medications prescribed for other conditions
Not everyone diagnosed with MASLD have any of the above risk factors, so it is likely there are other factors that contribute to the condition.
Will I experience any symptoms?
The majority of people who have mild MASLD will not notice any symptoms as the amount of fat build up in your liver is not enough to damage the liver.
Some people complain of tiredness and/or discomfort in the area surrounding your liver (on the right side of your body under your ribs). The discomfort may be as a result of extra fat build up causing your liver to expand resulting in the outer layer of your liver stretching causing the discomfort.
People who go on to develop NASH and cirrhosis may no experience symptoms for many years. The following symptoms could be because of development of your liver condition, and you must seek medical advice urgently:
- Yellowing of the eyes or skin (jaundice)
- Bruising easily
- Swelling of your tummy
- Vomiting blood
- Black, tarry stools
- Periods of confusion or poor memory
- Itchy skin
How is MASLD diagnosed?
For the majority of people, they only find out they have MASLD when they have routine bloods taken. You will be seen initially by your GP where they will ask you questions regarding your health and lifestyle and assess for risk factors associated with liver disease. Because your liver has many functions your GP may request further blood tests to help eliminate causes of liver disease by reviewing the pattern of your blood results.
You will be referred on to have a routine abdominal ultrasound scan to assist in diagnosing the health of your liver as well as a FibroScan if your blood results indicate it necessary. This is a non-invasive procedure which allows us to detect the level of fibrosis (scarring) in your liver which then enables us to determine how often you require further monitoring.
What treatments are available and what are the benefits of the treatment?
There are currently no specific medications available to prevent or treat MASLD, but there is lots of research into specific treatments currently underway. In some cases, your GP may focus on treating associated conditions such as obesity, diabetes, high blood pressure and high cholesterol as these conditions are also associated with MASLD.
Your GP will discuss any medications or treatments necessary with you prior to you commencing. If you would like more information about MASLD please go to www.britishlivertrust.org.uk or www.livernorth.org.uk
Looking after yourself
Alcohol
Alcohol can be consumed but you must adhere to safe alcohol levels of 14 units or less per week. If you have liver cirrhosis or advanced scarring of your liver, we advise abstinence from alcohol.
Diet and Exercise
There are no specific dietary or exercise requirements but maintaining a well-balanced healthy diet and adhering to regular exercise daily is essential to overall wellbeing and is recommended. To eat healthily you need to get the right balance between different foods. For most people, a well-balanced diet is one that is low in fat, sugar and salt, and high in fibre. Your diet should also contain enough protein and a wide range of vitamins and minerals. It is important to remember that your body’s nutritional needs may vary depending on the type and severity of your condition. Particularly, if you are unwell and losing weight you may need to vary your diet.
Please refer to www.britishlivertrust.org or www.livernorth.org.uk if you want more details on healthy diets associated with MASLD.
Will I need follow up appointments?
Once you have had your initial assessment with your GP and they have all your blood and ultrasound scan results back, you may require a FibroScan to determine the amount of scarring you have in your liver. You will be referred to the Queen Elizabeth Hospital for the scan and will receive an appointment letter via post informing you of the appointment date and time together with some information explaining what the scan entails. Depending on that result you will either be seen at the hospital every 6 months by one of the liver nurses or a doctor or discharged back to your GP with advice.
If you require a further FibroScan everyone or three years you will receive appointments in the post. A liver nurse will contact you by telephone within a couple of days of you having your scan to interpret the result for you and answer any questions you have regarding the next steps; you may receive your results during your scan appointment if a nurse is doing your scan.
What will happen if I do not attend an appointment/ telephone consultation?
If you do not attend your outpatient/telephone appointment you may be offered an alternative appointment or referred back to your GP. They will discuss with you whether you want to engage with the hospital for further appointments or if you would rather be followed up by your GP.
If I have any questions, who should I contact for advice?
You could contact one of the liver nurses via our hospital switchboard telephone 0191 482 0000 Mon to Fri 8:30 am until 4:30 pm, alternatively you could speak to your consultant’s secretary or seek the advice of your GP. Out of hours if you need to talk to someone about your appointment or any other issue which could not wait until the next working day during office hours you could contact the hospital switchboard and ask to speak to the senior nurse.
How to contact us?
If you need more advice or would just like to have a chat about your condition, please contact the liver nursing team via the hospital switchboard on Tel 0191 482 0000 or ring them on their direct line 0191 4453935.