IUI is a treatment used for the following fertility problems:
- Frozen partners sperm e.g., after cancer treatment
- Sexual intercourse problems
In order to offer this treatment, we must ensure the fallopian tubes are open, no more than mild or minimal endometriosis is evident and a reasonable sperm sample is obtained.
Treatment usually involves some stimulation with fertility drugs, depending on the woman’s natural ovulatory cycle. At ovulation time, a prepared sperm sample is deposited at the top of the uterus (womb) using a special catheter.
Prior to Treatment
In preparation for your treatment, you will be asked to complete some forms. You will be sent a SMS message to access your E Consent profile, and they must be completed in time for your consultation. These are from the Human Fertilisation and Embryology Authority (HFEA) and consist of:
- A registration form each
- Welfare of the Child forms for you each to complete
- Consent to disclosure for you both to complete.
- Consent for the gentleman to complete for the use of sperm in IUI treatment.
- Could you bring passports along that we can photocopy and place in your notes or NHS number and a passport photo of you both individually.
Prior to any appointments, both partners should have had blood tests for HIV, Hepatitis B & C. Ladies should also have an AMH test, and a semen analysis should have been performed for the men. It is essential these are performed prior to the consultation so the doctor can discuss the results. If these have not been obtained, please contact the unit as soon as possible.
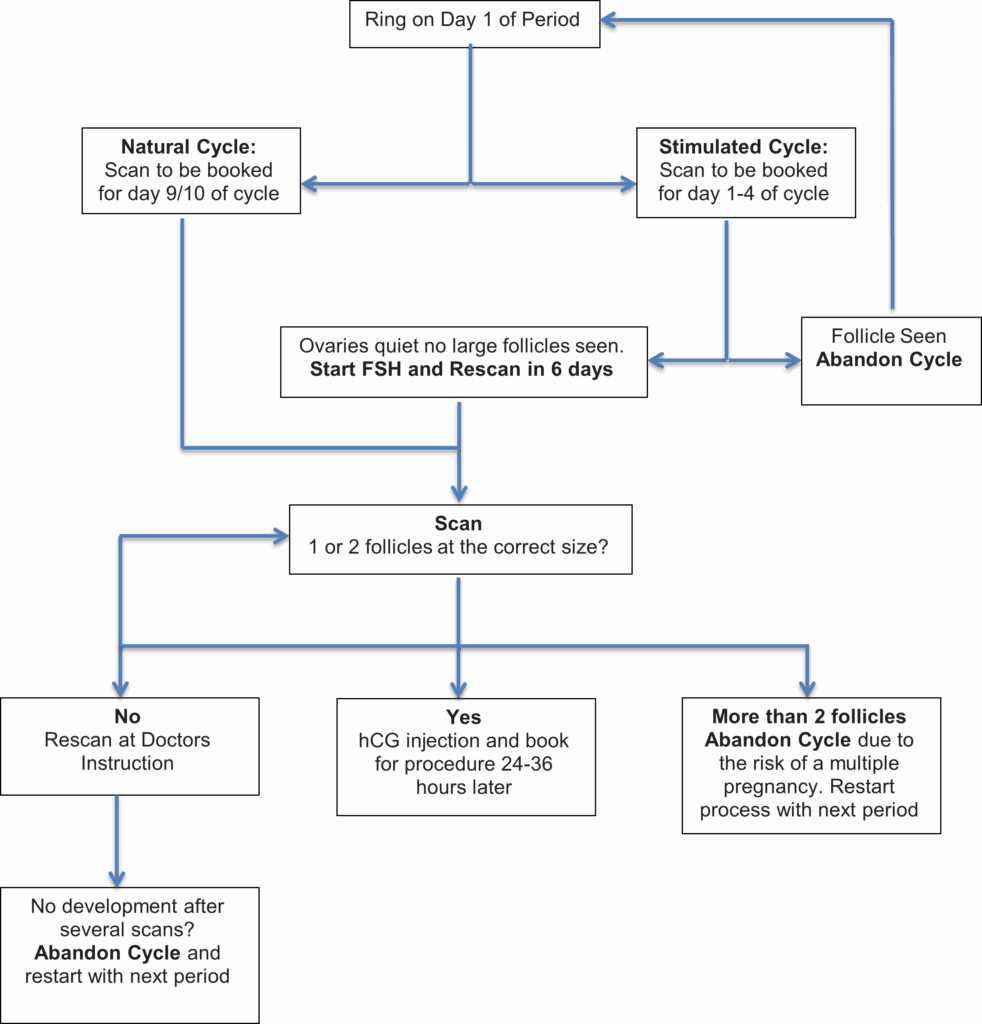
There are 2 different ways to prepare you for your insemination. This will be discussed at your consultation.
1. Natural Cycle:
Your cycle will be tracked using ultrasound scans until 1 or 2 follicles reach the correct size. Once this has been achieved an injection of human chorionic gonadotrophin (hCG) will be given to start ovulation.
2. Stimulated Cycle:
Fertility drugs (FSH) are used to stimulate the growth of 1-2 follicles and ultrasound scans allow us to monitor the growth of these follicles. Once the largest follicle reaches the correct size, an injection of human chorionic gonadotrophin (hCG) will be given to release the egg(s) from the follicle(s).
In both cycles the insemination will be performed between 24 -36 hours following hCG injection.
Your partner will need to give his sperm sample on the day of the insemination and the sperm will then be prepared.
The Procedure
IUI is a relatively painless procedure that is performed by the fertility nurses or one of the doctors. Using a speculum, the cervix is cleaned, and a fine catheter is passed through the cervix into the womb – this usually feels similar to a smear test. Next, the prepared sperm sample is placed into the womb through the catheter. You may feel some period-like cramps. After the procedure you will rest for at least 10-15 minutes before going home.
A urine pregnancy test is due 14 days after insemination, we will give you a pregnancy test to do at home. If you have a period, you can have another IUI cycle. If your pregnancy test is positive, we will arrange a blood test, and hopefully a pregnancy scans 2 weeks after your positive test and another scan 2 weeks after that.
We would generally offer 3 cycles of treatment and then review you however treatment may be reviewed earlier than this.
If you wish to discuss any aspect of your treatment, please don’t hesitate to approach a member of the unit team.
Step by Step:
Problems
Over Stimulation – occurs in 6-7% of patients taking fertility drugs. In such cases the treatment cycle will have to be abandoned to avoid high order multiple pregnancies.
Multiple Births – The use of fertility drugs increases the risk of a multiple pregnancy by 20-30% as more than one egg follicle may grow. The risk of multiple pregnancies depends on various factors.
The complications of pregnancy increase with multiple pregnancies:
- An increased risk of miscarriage and complications including raised blood pressure
- Higher incidence of premature birth. Babies born prematurely may have low birth weight and are at increased risk of still birth and perinatal mortality and if they do live, they may have serious disabilities, such as cerebral palsy and learning problems.
A multiple pregnancy can create the need for extended hospital stay both before and after birth.
Multiple pregnancy and birth can also have a potential strain not only physically but also emotionally, practically, and financially on a couple and any existing children.
To avoid this, cycles are strictly monitored by ultrasound scanning and if more than 3 follicles are developing, the cycle is abandoned.
Occasionally, no follicles may grow to be the size required to proceed with ovulation. In this situation, treatment would be abandoned, and you could restart with your next period. In subsequent cycles it may mean having a stimulated cycle rather than a natural cycle or increasing the dose of FSH in a stimulated cycle.
Contact Us
If you feel at any time that you are not happy with any aspect of your treatment, have concerns or would like to make a comment or suggestion and would like to discuss things further. Please do not hesitate to contact us as there will always be someone happy to help.
Telephone: 0191 445 2768 (direct line)
Email: [email protected]
or in the case of an EMERGENCY please call 0191 482 0000 and ask for the IVF Doctor on call after office hours.