What is an Intra-articular Joint Injection?
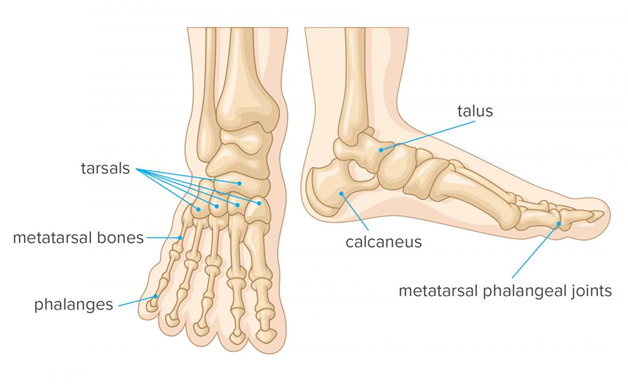
The foot and ankle is a complex structure made up of 33 joints, 26 bones and numerous muscles, tendons, blood vessels, ligaments and nerves. A joint is made where two or more bones join together and if these joints become inflamed it can cause pain, swelling and restriction movement which can affect your walking and daily tasks.
An intra-articular joint injection is a medical procedure in which a healthcare professional injects either a steroid, local anaesthetic or a combination of both directly into the joint, using x-rays to guide them. This is different to an injection that you may have on other parts of your foot or ankle to help with tendon pain. These injections do not need x-ray guidance so can be performed in the radiology department.
Intra-articular joint injections may be advised if all other non-operative treatments have been unsuccessful at helping you manage your symptoms or to help the healthcare professionals diagnose a source of pain.
Purpose of Intra-articular Joint Injections
In general, patients receive intra-articular joint injections for one of two reasons; to help manage their symptoms (Therapeutic) or to assist with a diagnosis (Diagnostic).
Steroid injections are used to help try reduce inflammation, which in turn aims to reduce the swelling and pain in the joint. The effect of the steroid injection may not occur immediately and can take a number of days or weeks before the pain relieving benefit is felt.
In some cases a local anaesthetic may be used. This aims to numb the nerves to the area inside the joint causing a painless sensation to occur. The benefit can be felt within 20-30 minutes of the injection being given. Local anaesthetics will only have a temporary effect.
What are the benefits of the procedure?
The temporary pain relief from an intra-articular joint injection may help:
- Reduce pain and inflammation
- Participation in physiotherapy
- Delay the need for surgery
- Confirm a diagnosis
Please note, if there are severe degenerative changes within the joint, the Intra-articular injection will have limited benefit.
What are the Contraindications of the procedure?
In some instances we are unable to perform an intra-articular joint injection, these include:
- Current infection / Sepsis
- Fracture
What are the Risks of the procedure?
As with all procedures there are some possible risks, some of which are minor, but some can be more serious. Specific risks to this procedure include, but are not limited to;
- Infection
- Bleeding
- Numbness to the area that is being injected, other parts of the foot or toes
- Nerve or Blood vessel damage
- Worsening joint pain or symptoms
- Allergic Reaction or Facial Flushing
- Skin changes near to the injection site
- Failure to improve symptoms
- Progression of Osteoarthritis
Please note, if you are currently taking any blood thinning medication (such as Warfarin), it might further increase the risk of bleeding, therefore may need to be stopped 5-7 days prior to the injection.
How long will I be in hospital?
The procedure is usually carried out as a day case, either in Theatre or the X-ray Department. This means that you will usually be in hospital for half a day.
Preparation for the Injection
In order to help reduce the risk of infection it is important to keep the skin clean and free from open wounds. Please use the antimicrobial wash (Octenisan) 5 days leading up to your injection. Please check to see if you need to stop any medication prior to attending the hospital.
What to expect on the day of the procedure
On arrival you will be seen by the Practitioner or Doctor carrying out the procedure who will discuss the procedure with you. If you have not done so already you will be asked to sign a consent form and a small arrow is drawn on the skin close to the injection site.
X-rays will be taken during the procedure. The injection itself will only takes a few minutes, but the overall procedure may take approximately 20 minutes. The Practitioner or Doctor will use x-ray guidance (fluoroscopy) to direct a needle into the joint. Once correct placement is confirmed the injection solution is slowly administered. Following the injection a small dressing will be applied to the area.
Once the procedure is completed you will be monitored for approximately 20-30 minutes. You will then be discharged with an advice leaflet. You will be unable to drive home after the procedure so it will be necessary for you to make arrangements for transport home. It is advisable to avoid excessive exercise involving the joint for 24 hours following the procedure. It is advisable to continue taking your pain relieving tablets until the injection begins to take effect.
The amount of pain relief and the length of time it lasts is different for everyone. After a period of time an injection may be repeated, but this decision is at the discretion of the Consultant team.
Some Consultants may want to avoid proceeding with surgery for 3-6 months following an intra-articular joint injection.
When to seek medical attention
We would advise you to seek medical help if you experience any of the following after the injection:
- High fever
- Swelling
- Redness and/or drainage from the injection side
- Severe pain.
Follow up
The follow up plan is different between each Consultant. You will either be seen face to face in the Orthopaedic Clinic or receive a telephone appointment after the injection to re-assess your symptoms and make a plan of future management.
How do I make a comment about my visit?
We aim to provide the best possible service and staff will be happy to answer any of the questions you may have.
If you have any suggestions or comments about your visit, please either speak to a member of staff or contact the patient advice and liaison service (PALS) on 0191 445 6129 (09.00 – 17.00, Monday to Friday).
You can also email PALS at [email protected]
Alternatively, you may wish to complain by contacting our complaints department:
Mrs Trudie Davies,
Gateshead Health NHS Foundation Trust,
Trust Headquarters,
Queen Elizabeth Hospital,
Sheriff Hill,
Gateshead,
NE9 6SX
The PALS team will listen to your concerns, suggestions or queries and is often able to help solve problems on your behalf.
| Telephone numbers | |
| During the hours of 8am – 8pm contact the Orthopaedic Secretaries | 0191 445 8500 |
| During the hours of 8pm – 8am contact Ward 28, Queen Elizabeth Hospital. | 0191 445 2028 |
| Main Hospital Switchboard | 0191 482 0000 |
Data Protection
Any personal information is kept confidential. There may be occasions where your information needs to be shared with other care professionals to ensure you receive the best care possible.
In order to assist us to improve the services available, your information may be used for clinical audit, research, teaching and anonymised for National NHS Reviews and Statistics.
Further information is available via Gateshead Health NHS Foundation Trust website (Privacy – Gateshead Health) or by contacting the Data Protection Officer by telephone on 0191 445 8418 or by email [email protected].
This leaflet can be made available in other languages and formats upon request