This booklet has been produced by the Trauma and Orthopaedic Department. It is designed to provide information about hip arthroscopy and what to expect before and after the operation.
This advice is provided to assist with shared decision making when singing informed consent for surgery and help to prepare you for surgery, and the expectations of recovery and rehabilitation. It is recommended that you read this booklet before your surgery and write down any questions you may have. You should bring it with you when you come to the hospital.
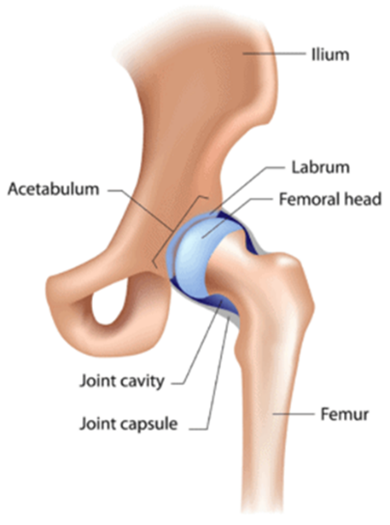
Anatomy
The hip is a ball-and-socket joint that is surrounded by a watertight capsule. The socket is formed by the acetabulum, which is part of the large pelvis bone. The ball is the femoral head, which is the upper end of the femur (thighbone).
A slippery tissue called articular cartilage covers the surface of the ball and the socket. It creates a smooth, frictionless surface that helps the bones glide easily across each other.
The acetabulum is ringed by strong fibrocartilage called the labrum. The labrum forms a gasket around the socket.
The joint is surrounded by bands of tissue called ligaments. They form a capsule that holds the joint together. The under surface of the capsule is lined by a thin membrane called the synovium. It produces synovial fluid that lubricates the hip joint.
What is a Hip Arthroscopy?
Arthroscopy is a form of keyhole surgery in which a camera is used to look inside a joint. To do this effectively the surgeon will use traction (a pulling force) to bring the hip slightly out of joint, allowing the surgeon to get a good view of the hip and any areas that are causing your symptoms. In order to perform the operation, the surgeon will make a small cut (incision) through which a camera is inserted. This will enable the surgeon to look inside your hip. Several other incisions of the same size may be required in order to insert other instruments to deal with your hip problem.
What is a Hip Arthroscopy used to treat?
Hip arthroscopy can be used to treat many problems in the hip joint with the benefit of being less invasive than other hip joint operations. There are many conditions that may be treated with hip arthroscopy. The most common conditions treated with hip arthroscopy are:
- Femoroacetabular impingement (FAI) – This condition involves the head of the thighbone (femur) and the rim of the socket (acetabulum). The condition is caused by a different shape of the femoral head (Cam) or of the socket (Pincer) causing abnormal contact. This may cause pain in the hip joint during certain movements or positions. An arthroscopy can be used to reshape the femoral head and socket to prevent this abnormal contact.

- Labral tear – The hip socket has a rim of fibrous cartilage called the labrum. This cartilage can be injured because of abnormal contact or through other causes. An arthroscopy can be used to repair or remove part of this tissue.
What are the benefits of hip arthroscopy?
- Improve function of the hip joint
- Help to reduce pain
- Restore joint mechanics
- Delay / stop progression of disease
What are the alternative treatment options?
- Pain relief
- Physiotherapy rehabilitation
- Modification of activities
- Nonsteroidal anti-inflammatory medication
- Corticosteroid injection into the hip joint
What are the risks / complications which could occur?
All surgeries have a potential for complications and whilst this section is not intended to scare you as a patient, it provides information to help you to make an informed decision in the consent process.
It is important that you understand the possible risks linked with any major operation.
Your surgeon or the member of the orthopaedic team will discuss the operation during the consent process and typically would list the following potential complications on the consent form, “pain, infection, fracture, bleeding, thromboembolism, nerve damage, heterotopic ossification, avascular necrosis, further surgery and risks to limb or life”. You will be asked to sign the consent form stating that you understand and are accepting the risks when undergoing surgery. You can withdraw from surgery at any point of time if you have changed your mind.
- Pain – Pain can happen with any operation. A local anaesthetic is given during surgery to help control your post-operative pain and you will have pain relief to go home with. You might still experience pain postoperatively but that will reduce in time as you progress with your recovery.
- Infection – Risk is less than 1%. Keep your wound dry and covered. Let the healthcare team know if you get high temperature, notice pus in your wound, or if your wound becomes red, sore or painful. An infection usually settles with antibiotics, but you may need special dressings and your wound may take some time to heal. In some cases, another operation might be needed.
- Bleeding
- Blood clots – Deep Vein Thrombosis – DVT. This can cause pain, swelling or redness in your leg, or the veins near the surface of your leg to appear larger than normal.
- Pulmonary Embolism – PE. This is the term used for a blood clot in the lung and symptoms consist of shortness of breath, chest pain, increased heart rate and blood in your phlegm. To prevent the blood clots accruing during or after the surgery you might be given blood thinning medication, compression stocking to wear or inflatable boots. Please inform healthcare team if you think you might have a blood clot.
- Nerve damage around the hip could lead to numbness, weakness and pain in your leg or foot. Risk is 1 in 250. This usually gets better in time but may be permanent. When traction is used during the operation to pull your hip apart, the pudendal nerve in your groin can be damaged. This can cause numbness in your groin. For men, it can sometimes cause problems having an erection. The nerve usually recovers in a few weeks.
- Bone forming in muscle around your hip (heterotopic ossification). Risk is 1 in 20.
- Injury to articular cartilage
- Under or over correction
- Hip dislocation
- Avascular necrosis (AVN)
- Femoral fracture
- Compartment syndrome can occur as a result of increased pressure around the muscles of the lower leg as a consequence of bleeding or swelling, requiring emergency pressure relieving operation.
- Failure to improve symptoms / further surgery.
How long will I be in hospital?
A hip arthroscopy is a planned day case procedure; therefore most patients will be discharged on the day of surgery.
You will only be discharged when you are medically safe to do so.
What to expect on the day of surgery?
On coming into hospital a member of the team will welcome you. The nurses will look after you and answer any questions you may have. You will be asked to change into a theatre gown.
The surgeon and anaesthetist will visit you and answer any questions that you have. If you have not done so already, you will be asked to sign a consent form. A nurse will go with you to the anaesthetic room and stay with you until you are asleep.
A cuff will be put on your arm, some leads placed on your chest, and a clip attached to your finger. This will allow the anaesthetist to check your heart rate, blood pressure and oxygen levels during the operation. A needle may be put into the back of your hand to give you the drugs to send you to sleep.
What happens after the operation?
A nurse will check your blood pressure, pulse and the area where the operation has been done. You will normally be able to have a drink shortly after the procedure and eat as soon as you feel hungry.
You can usually get out of bed an hour or so after you wake up and you should wait for the nurses to help you as you may feel a little dizzy at first. It is likely to be a bit painful where the operation has been carried out, but if you move carefully, the pain is usually limited. The nurses will monitor your pain and give you painkillers, if necessary. It is quite normal for a small amount of blood to soak through the dressing and this can easily be changed. Sometimes the staff will need to press gently on the dressing for a while to prevent this happening again.
Recovery after surgery
Your hip will feel painful and swollen after the arthroscopy, this is normal. It is important to be aware of your pain level. Take your pain relief regularly, as prescribed by the hospital. A clinic appointment will be made for you to see a member of the lower limb orthopaedic team in the coming weeks after surgery.
Walking
Unless you have any restrictions you must try to walk normally as soon as you can. You may need to use crutches for a few days/weeks to help you walk without a limp. Please remember to return the walking aids when you no longer need them.
If you’re post-operative instructions include a change to your weight baring status, this will be explained to you by the physiotherapist before you are discharged.
Swelling
Swelling and inflammation is a normal part of the healing process. Dependant on your surgery this can last up to a few months. Swelling of the leg is different for everyone and may cause the leg to ache and feel very heavy.
Following your discharge from hospital; you need to apply the ice pack three to four times daily for 15-20 minutes. You will be able to reduce the frequency after this time but will find that you will benefit from ice therapy for up to three months to help manage the swelling.
Work
You should return when you feel able to cope with the physical demands of your job. You can discuss this with your GP or Consultant if you are not sure.
Driving
After a hip arthroscopy it is advisory that you do not drive until you can walk normally without crutches. It is also required that you feel safe behind the wheel and safely perform an emergency stop. We also advise you to inform your car insurance company of your recent hip surgery.
Physiotherapy
An appointment will be arranged to your appropriate outpatient physiotherapy service upon discharge from hospital. It is advised that you engage with the advice and exercise you are given when leaving hospital.