Why have I been provided with this leaflet?
A polyp has been found in your stomach and we would recommend removal for precautionary measures. This leaflet explains to you more about your condition and what is involved in its treatment.
What is a gastric polyp?
A polyp is a small growth that sometimes forms on the lining of the stomach. Most small polyps are harmless but if they are left to grow into large polyps they can become cancerous.
Larger polyps (more than 2cms) have a small chance (1 in 10 or 10%) of having cancerous cells. We can still remove these polyps as part of your endoscopic procedure and this may be all that is required. Occasionally it is not possible to remove some large polyps this way and therefore an operation may be required. Most polyps do not cause any symptoms but in some cases they can cause bleeding or a change in stomach habit.
Why have I been referred to the complex polyp service?
The removal of larger polyps carries greater risk of unplanned events including bleeding or perforation. The complex polyp service undertakes these procedures on a regular basis and hence has the experience to reduce the chance of such events.
What are the benefits?
There is a small but significant chance that there are cancerous cells in your polyp. Polyps usually grow and may remain benign or they may turn into a cancer in the future. For this reason we recommend removal of the polyp to identify cancer early and to prevent cancer occurring later. Large polyps can cause symptoms and removing them can improve your quality of life.
How do we remove large polyps endoscopically?
Endoscopic removal of larger polyps takes longer than a standard or diagnostic gastroscopy but this can vary depending on the size and position of the polyp. For this reason we usually remove the polyp under general anaesthetic in theatre.
There are two ways that we can remove a gastric polyp endoscopically. Endoscopic mucosal resection (EMR) and Endoscopic Submucosal Dissection (ESD).
Endoscopic mucosal resection (EMR)
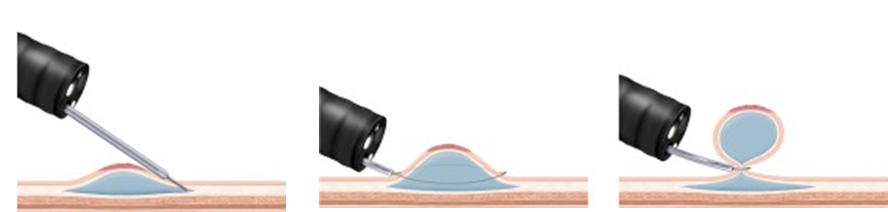
The Endoscopist will firstly use the endoscope (camera) to find the polyp. Next a special needle is passed through the camera and inserted into the base of the polyp as shown below. Fluid is injected through the needle to raise the polyp away from the stomach wall. A wire snare is then passed through the camera and positioned around the raised polyp. The snare is pulled tight and an electric current is passed through the snare which burns any blood vessels as the polyp is cut off. If the polyp is very large, it may be removed in a number of pieces in the same way. Once the polyp has been removed, it is retrieved so that it can be sent to the pathology lab for further analysis.
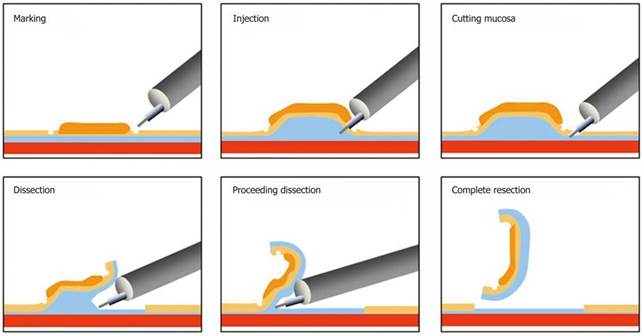
Endoscopic Submucosal Dissection (ESD)
The Endoscopist finds the polyp as before. Then a special tool is used to carefully cut around and underneath the base of the polyp This takes time and slowly the polyp is peeled off from the stomach wall and finally it can be removed in one piece. If the polyp is in one piece we can usually tell how deep any cancerous cells reach if they are present. This will give you the best risk assessment of any spread of the cancerous cells outside of the stomach.
What are the risks of removing large polyps?
Endoscopic removal of gastric polyps is generally very safe but there are risks.
The main risks are:
- Perforation – this means a tear in the stomach wall. For EMR, this occurs about once in every 100 patients (1%). For ESD the risk is up to 1 in 20 (5%). Perforation can occur up to 14 days after the test. Perforations can heal with readmission and strong antibiotics and usually they can be treated with the endoscope. However sometimes an emergency operation is required.
- Bleeding – bleeding may occur once in 2 – 5 out of 100 patients (2-5%). Bleeding can occur up to 14 days after the procedure. Blood transfusion or further endoscopies may be required. Very rarely emergency surgery may be needed to stop it. If you have a condition which may increase your risk of bleeding such as Haemophilia, von Willebrands disease or low platelets please inform the endoscopy department.
- Incomplete removal – sometimes the Endoscopist cannot remove the entire polyp the reason for this will be discussed with you after your procedure – if this happens, you may need a further attempt using the endoscope or an operation might be planned at a later date.
- Recurrence– even when all the parts of the polyp visualized on the camera are completely removed the polyp can come back in the same location. This is called recurrence. Depending on the nature of the polyp this can happen in up to 10% of patients. Usually this can be dealt with by a repeat camera test undertaken in three months. Sometimes the recurrence may be persistent needing more than 1 attempt at treatment three months apart
- General Anaesthetic– You can have complications related to anaesthetic, we aim to reduce this risk by assessing your general health prior to the endoscopy procedure and you will be closely monitored by qualified staff during and after the examination.
What happens if the endoscopist does not think that EMR or ESD is possible?
In this case, you will usually be seen in clinic and the doctor will discuss whether you need to have an operation to remove the polyp.
Are there any other ways of dealing with my polyp?
There are two main alternatives to having an endoscopic removal of your polyp in theatre:
- We could decide to leave the polyp as it is and do nothing. This option may be preferable in patients who have significant health problems. The rationale being that the polyp is unlikely to cause problems in the patient’s lifetime.
- The polyp could be removed by having an operation on the stomach. This is usually a straight forward procedure which may be an open or key-hole procedure but carries the risks of general anaesthetic and surgical complications such as infection and delayed healing. The risks of surgery may be considerably higher if you have other medical conditions.
These options will be discussed with you in detail at your pre assessment appointment and by the Endoscopist undertaking the procedure.
After the examination
You will be admitted to the ward for overnight stay after your procedure for monitoring purposes. This is usually for your own safety and you should be allowed home the next day.
How will I know the results of my test?
The Endoscopist performing the procedure will often be able to give you some results straight after the procedure. Before you are discharged from the ward you will be given clear details concerning follow up arrangements and aftercare information. A full report will be sent to your GP and/or hospital consultant. You will be given contact details in the event of any complications that may occur. After two weeks there is little or no chance of any complications post polypectomy.
The polyp is usually retrieved during the Endoscopic procedure and sent to the pathology laboratory for further analysis. It can take up to two weeks before a result is available. Your consultant will then be in touch with you regarding these results. Sometimes decisions about further treatment can only be made once these results are available.
Contact numbers
If you have any further questions, you should contact the following:
Queen Elizabeth Hospital (main switch) 0191 482 0000
Out of hours
Accident and Emergency 0191 445 2171
Endoscopy
Endoscopy department
Queen Elizabeth Hospital
Sherriff Hill
Gateshead
Tyne and Wear
NE9 6SX