This booklet is for patients who have had knee replacement surgery at Gateshead Health NHS Foundation Trust.
Inpatient length of stay
We aim to get you home as soon as possible following surgery once all discharge goals have been achieved and you are medically well. This is usually 1-2 nights after surgery.
Goals of initial rehabilitation:
- Restore knee range of movement:
- Bending the knee to 90 degrees and being able to straighten the knee.
- Regain thigh strength
- Reduce swelling
- Adequate pain control
Discomfort
Post-operative pain, swelling, and bruising are a normal part of the recovery process following joint replacement surgery. The muscles and tissues surrounding your knee will take time to heal. You will require pain relief medication on a reducing basis, usually over at least 6 weeks following the surgery. Crutch use, ice, activity pacing and rest may help.
Increased discomfort at night and difficulty sleeping is very common following a knee replacement, this should improve with time.
Following your discharge from hospital; you need to apply the ice pack three to four times daily for 15-20 minutes. You will be able to reduce the frequency after this time but will find that you will benefit from ice therapy for up to three months to help manage the pain.
If you have any concerns regarding managing your pain, please discuss this with your GP.
Swelling
Swelling and inflammation is a normal part of the healing process. This can last up to a few months or longer but will improve with time. Swelling of the leg is different for everyone and may cause the leg to ache and feel very heavy. It is common for the knee to remain slightly larger following a knee replacement.
Elevating your leg on a stool or on the bed will also help manage the swelling. Do not rest a pillow underneath your knee in a semi bent position. Although this may feel comfortable, it may cause problems with your movement and walking pattern.
When should I seek help?
You should see your doctor urgently if you:
- Have a sudden increase in severe pain, swelling or tenderness in the calf which is getting worse and not just related to pain expected while performing the exercises.
- Have concerning pain, swelling or tenderness in the joint which is getting worse.
- Develop a high temperature and feel unwell.
- See fluid, pus or blood coming from the wound.
- Develop new numbness or tingling near to the joint.
Mobility and Walking Aids
After your operation, it may be necessary for you to use crutches to help you walk. Your physiotherapist will provide you with a pair of crutches and show you how to use them.
Everyone is different as to when they stop using crutches; this often depends on your previous level of mobility. When you feel confident with your elbow crutches and you are able to walk without a limp, it is recommended you progress to using only one crutch in the hand on the opposite side of your surgery.
For example: if you have a left knee replacement, use your elbow crutch/stick in your right hand.
Once you are no longer using your crutches; please return them to the hospital. You will be provided with further guidance from the outpatient physiotherapy staff as to when it is appropriate to gradually stop using elbow crutches.
Stairs / Steps
Going up stairs with a rail
Keep your crutch/es on the step you are standing on.
Step up with your un-operated leg, then your operated leg and then bring your crutch/es up onto the same step.

Going down stairs with a rail
Put your crutch/es down first into the middle of the step below. Step down with your operated leg and then follow by your un-operated leg.

Going up stairs without a rail
Keep your crutches on the step you are standing on.
Step up with your un-operated leg, then your operated leg and then bring your crutches up onto the same step.

Going down stairs without a rail
Put your crutches down first into the middle of the step below. Step down with your operated leg and then follow by your un-operated leg.

Exercises
It is important that you continue doing the exercises that have been given to you by the physiotherapist on the ward. These exercises should be completed three to four times a day.
It is normal to experience additional discomfort whilst doing these exercises and for up to an hour afterwards.
Prior to commencing exercise, it is advisable to take adequate pain relief to optimise the benefit of these exercises. Especially if you are finding them difficult. Then use ice following completing your exercises.
Static Quads
Pulling your foot towards you and push your knee downward against the bed.
Hold for 5-10 seconds, Repeat 10 times, 3-4 times a day

Straight Leg Raise
Straighten your operated leg, pull your toes towards you and lift your leg to about 2 inches above the bed.
Hold for 5-10 seconds, Repeat 10 times, 3-4 times a day

Inner Range Quads
Lie on your back, place a firm cushion or towel under you operated leg, pull your toes towards you, push down onto the cushion/towel and lift the lower part of your leg off the bed.
Hold for 5-10 seconds, Repeat 10 times, 3-4 times a day
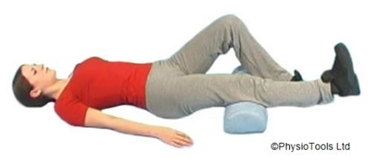
End Range Extension
Place a rolled towel under your ankle. Straighten your knee by tightening your thigh muscles. Try to touch the bed with the back of your knee.
Hold for 10-15 seconds, Repeat 10 times, 3-4 times a day

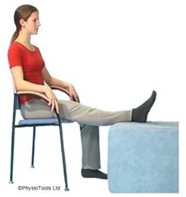
Seated Quads
Sit in a chair, pull your toes up towards you and tighten your thigh muscles to straighten your knee slowly.
Hold for 5-10 seconds, Repeat 10 times, 3-4 times a day

Knee Bends
Whilst sitting with your thigh supported, slowly bend your knee as far as you can. If this is too uncomfortable or to increase the stretch; you can control the bend with your other foot.
Hold for 15-20 seconds, Repeat 5 times, 3-4 times a day

Gravity Assisted Passive Extension
If you are struggling to get you knee fully straight, you will benefit from leaving your knee in passive extension. Whilst you are sitting, rest with your heel on a pillow or stool without the back of your knee supported for as long as tolerated.
Please follow the link to watch ‘Joint Care Clinic – Knee Exercises’
Outpatient Physiotherapy
Once you have left hospital, you will receive outpatient physiotherapy rehabilitation. You should receive your appointments to attend outpatient physiotherapy via post after you leave hospital. This will be approximately two weeks after discharge.
If you are a registered patient of a Gateshead or Newcastle GP, the Tyneside Integrated Musculoskeletal Service (TIMS) will be your physiotherapy provider: https://www.tims.nhs.uk / 0191 445 2643
If you are a registered patient of Durham GP, the County Durham integrated MSK service will be your physiotherapy provider: https://patient.inhealthcare.co.uk/selfenrol/v2/form / 01388 455 200.
If you are an out of area resident (Registered to a GP out of Newcastle/Gateshead/Durham) the Queen Elizabeth Hospital physiotherapy team will be your provider: https://www.gatesheadhealth.nhs.uk/services/physiotherapy/musculoskeletal-physiotherapy-service / 0191 445 2320.
It is important that you attend outpatient physiotherapy.
At this appointment the physiotherapist will:
- Assess the progress you have made since your discharge from the ward.
- Progress and guide on exercises.
- Assess your walking and progress to the most appropriate walking aid.
- Answer any queries you may have.
Follow up appointments can be arranged for physiotherapy at this appointment if the therapist feels it is necessary.
Please note: If you have not received notification of your follow up physiotherapy appointment/s within 2 weeks of leaving hospital, please ring 0191 445 2320 so we can check your referral.
On attending outpatient physiotherapy please wear comfortable clothing/ footwear that is suitable for exercise.
Follow up
You will have an appointment in the orthopaedic clinic 6-8 weeks after your procedure.
Transport
If you require an ambulance for transport to the group; you will be provided with a telephone number to ring and arrange this. This will be sent out with your physiotherapy appointment letter.
Community Rehabilitation
Occasionally people are discharged home using a walking frame. If appropriate; the ward physiotherapist may need to make a referral to the community team to review and progress rehabilitation at home. You will be contacted by either telephone or letter to advise when a visit can be arranged.
Please note: If you have not received notification of your follow up physiotherapy appointment/s within 2 weeks of leaving hospital, please ring 0191 445 2320 so we can check your referral.
Work
Returning to work will be dependent on the demands of your job. This will be guided by your surgical team and physiotherapist. This will be sooner if you have a sedentary / desk based job. If you have a heavy manual job you may require longer off work. You can discuss this with your GP or Consultant if you are not sure.
Driving
You will not be able to drive for at least 6 weeks following your operation. Once you are able to walk without any mobility aids you can drive when you feel safe to do an emergency stop and safely control a car. You must tell your insurance company that you have had knee surgery. If in doubt, contact your consultant or GP.
Telephone Numbers
If you are at all worried by your knee please contact us:
| During the hours of 8am – 8pm contact the Orthopaedic secretaries | 0191 445 8500 |
| During the hours of 8pm – 8am contact the Peter Smith Surgery centre, Queen Elizabeth Hospital | 0191 445 2028 |
| During the hours of 0800 – 16:30 contact the Physiotherapy Department | 0191 445 2320 |
| During the hours of 8am-8pm. If you have a Gateshead or Newcastle GP, the TIMS will be your physiotherapy provider. If you have a query about your first appointment with TIMS please contact our booking team on 0191 445 2643 If you are a current TIMS patient and have a query about your follow-up appointment please contact our local admin team on 0191 213 8800 | Booking Team: 0191 445 2643 Local Admin Team: 0191 213 8800 https://www.tims.nhs.uk/ |
| During the hours of 8.30am-12pm and 1-4pm. If you have a Durham GP, the County Durham Integrated MSK Service will be your physiotherapy provider. | Central booking team: 01388 455 200 |
| Main Switchboard | 0191 482 0000 |