This manual is designed to help you recover in the quickest and safest way. It also has valuable information for relatives and friends of those recovering from critical illness as it is recognised that you are very much involved in the process of recovery. It has been written using research and information, some of which was provided by patients who have previously been in critical care.
The manual is divided into three parts:
Part one will provide you with information about the critical care department and some common problems that may occur.
Part two provides information about what you can do to help with these common problems. If you live with someone, let them read the information with you, it can help them understand what has happened.
Part three contains useful information on national and local support services and guidance on exercise.
On this page
- What is the Critical Care Department?
- The Equipment in Critical Care
- Rehabilitation whilst in critical care
- Transfer to the Ward
- The Changing Environment
- The Change in Staffing
- The Change in You
- Planning Recovery
- Useful Contacts
- Discharge Home
- Introduction to Recovery
- Sleeping
- Vivid dreams and delirium
- Changes in Mood
- Anxiety
- Signs and Symptoms of Anxiety
- The vicious cycle of anxiety
- Depression
- Signs and Symptoms of Depression
- Diarrhoea
- Memory loss
- Getting back to normal
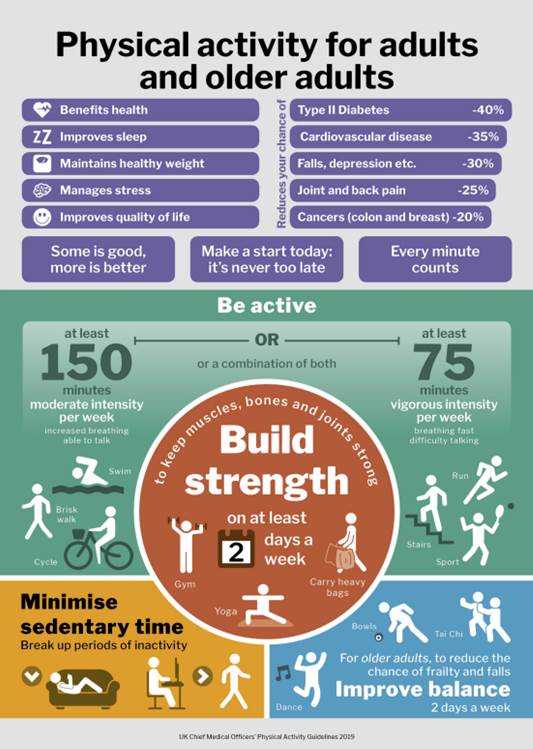
- Exercise
- Relaxation techniques
- How to get started
- How to relax
- Eating Normally Again
- Sex after Critical Illness
- Lifestyle Changes
- Useful telephone numbers
- National Support Groups and websites for information
- Drugs
- Local Support Services
- Exercise Plan
- Chair based exercise
- General advice on 8 ways to get active every day
Part One – Information
What is the Critical Care Department?
The critical care department is a ward within our hospital that cares for patients whose conditions are life-threatening and need constant, close monitoring and support from equipment and medication to keep normal body functions going. Due to the specialist treatments and the constant monitoring that patients require on critical care, it has a higher level of staffing. The staff who work here are highly trained in caring for the most severely ill patients.
Level three (also known as intensive care) is where patients who are requiring the most intense levels of care are looked after. These patients have one nurse looking after them all the time. Level two (also known as high dependency) is where patients go when they are needing less intensive care and one nurse looks after two patients in this area. These two areas are both part of the critical care department.

The Equipment in Critical Care
The equipment in a critical care area can seem frightening at first. It is common for patients to be connected to several different machines or devices if they are critically ill. As patients recover the equipment is slowly removed as it is no longer needed.

A monitor is positioned by each bedside and records heart rate, blood pressure and oxygen levels in the blood. For this to work you will need to be connected to a number of leads. The monitors beep to draw the attention of a nurse to check your condition. You may remember hearing these alarms.
Infusion pumps are used to give drugs and fluids through drips into the veins. Sometimes this is through a line in your neck called a central line (see picture below).You may have also had an arterial line in your wrist which is used to take blood samples and monitor your blood pressure.

You may have required assistance with your breathing through ‘non-invasive’ methods. This can be in the form of a tight mask over your nose and mouth, this is called a non-invasive mask sometimes called ‘NIV’. Another form of this type of help with breathing is called high flow oxygen which comes through nasal cannula which are small tubes which go up your nose.


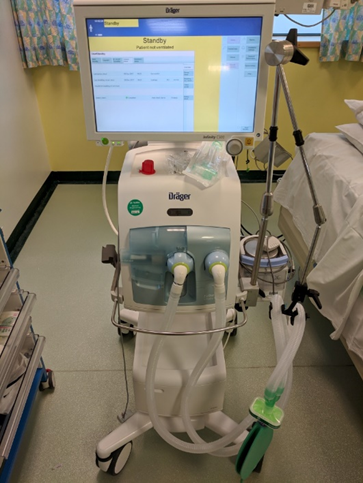
This is a kidney filtration (CVVH) or dialysis machine which can be used if your kidneys are not working normally. This works in a similar way to a dialysis machine, which removes waste from the blood and manages fluid levels. Blood circulates from the body through the dialysis machine, where it is filtered and then returned to the body.

Rehabilitation whilst in critical care
If you have required non-invasive help with your breathing it is really important to get up and moving as soon as possible. The staff on critical care will encourage you to get out of bed and sit in a chair. They will also encourage you to get up on your feet and walk as soon as possible.
It is important to get into your own clothes as soon as is practical, the nursing staff will guide you as to when this is appropriate. Where possible the staff may offer to take you out of the department for a change of scenery. To try and maintain your normal routine your family can bring in any papers you might like to read, books, tablet computers or any other activities you might enjoy.
Transfer to the Ward
The decision for you to leave critical care ultimately rests with the critical care consultant, but these decisions are made in close consultation with the nurses and doctors on the critical care team and the specialist teams involved (surgical or medical). When you are transferred to the ward there is a detailed handover between the critical care nurses and the ward nurses and between the medical teams.
Leaving critical care should be a time for celebration. You are getting better and are well enough to no longer need the high levels of care. However, we acknowledge this can be a very difficult time for you and your family, particularly if your admission to critical care has been long. No matter how much preparation has been done, patients will find a difference in the level of care between the critical care area and general wards.
You will find it useful to be more acquainted with your nurse call bell which is generally a white handset with an orange button. You must use this to alert the attention of one of the team if you are in pain, need to go to the toilet or if you have any other concerns. Do not hesitate to use it as the staff are there to help you at all times.
Some of the key issues patients face when being transferred to the ward are:
- The changing environment
- The change in staffing
- The change in yourself
The Changing Environment
Although critical care can be a difficult place to be, for some patients it is a safe place to be, it is a big change going to a ward. The daily routines are different, the staff are different, the sounds are different. The other patients are likely to be well enough to talk to you, this is very different from critical care. Some patients on the ward may be confused or noisy and this can be very disturbing. Most of the beeps and noises from the machines in critical care will have stopped, these beeps and alarms will often have become familiar and their absence can be just as worrying for some patients.
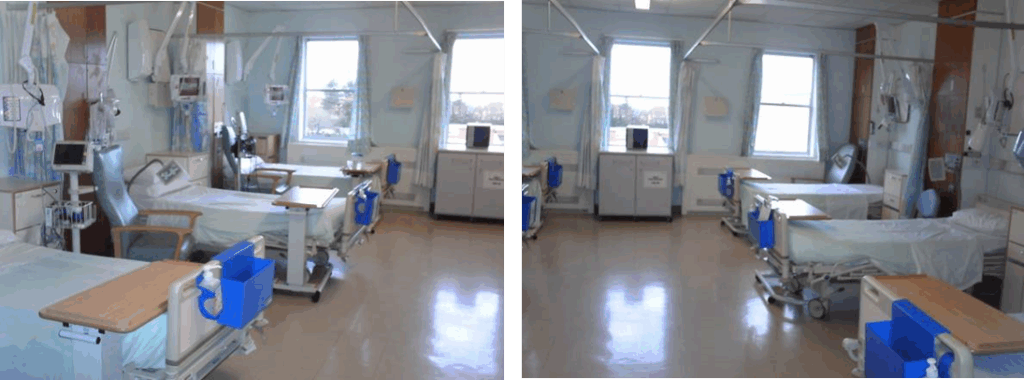
Some of the medical and surgical wards in our hospital are made up of four bays with four to five beds in a bay. Each bay will be allocated to either males or females. There are also wards which are made up of all individual cubicles. Some wards have a combination of bays and cubicles.
Visiting times vary on the wards in the hospital. Information on these times can be found at www.gatesheadhealth.nhs.uk or you can speak to one of the nursing staff to find out.
The Change in Staffing
In critical care there is usually one nurse per patient or one nurse for two patients depending on the level of care required. On a ward there will be two or three nurses for the whole ward along with a number of nursing assistants. You will be given a call bell to attract the attention of the staff, sometimes there may be delays in someone responding. This is due to the number of patients on a ward and the nursing demands at that time.
The thought of transferring to the ward can be frightening to some; however this is a really positive step in your journey of recovery. You are no longer requiring the high levels of care you received in critical care as your condition has improved. The medical and nursing staff will be very happy to update you on your condition at your request.
The Change in You
The process of recovery from critical illness is not easy. Going back to the ward often means you are becoming more independent, and this can be very hard work and tiring. Learning to eat and swallow normally again, getting washed and dressed, and going to the toilet normally are far from trivial tasks. Setting small realistic goals with the rehabilitation team will help you to reach your target.
Planning Recovery
When you go to the ward a member of the site resilience team will come and review you within the first twelve hours. The team is made up of senior nurses with advanced clinical skills and experience. They will review your condition and progress and if necessary they will address any specific issues.
If required our Rehabilitation Assistants will visit you every day whilst you are in hospital. Their role is to promote independence with hygiene and dressing, to support you in your exercise program and assist with mobility. The Specialist nurse will also visit you several times a week and will carry out health checks, identify any problems you may be facing because of your illness, liaise with the multidisciplinary team and help you achieve your rehabilitation goals so that you can recover as quickly as possible. The whole team would like to support you in your recovery from critical illness, make it as smooth as possible and answer any questions you may have.
Useful Contacts
Your Rehabilitation contact is …………………………………………..
If you have any problems or you are worried about anything following Critical Care you or your family can contact the critical care rehabilitation team on 0191 4453210.
There is an answerphone so we will endeavour to answer your call within 24 hours.
Discharge Home
The decision for you to be discharged from hospital will ultimately be made by your medical or surgical consultant. However these decisions are made in close consultation with other members of the team who have been taking care of you during your recovery including, nursing staff, physiotherapy, occupational therapy and dieticians.
The support that you may require when you are discharged will vary depending on many factors. Once you have been discharged home from hospital you will have already progressed significantly in your recovery. However, it may take several months until your physical strength is back to normal and the emotional impact of having been critically ill can last for some time. This recovery phase may be difficult for you and your family which may lead to some anxiety and low mood at times but this is quite normal.
Part two – What you can do to help yourself
Introduction to Recovery
When you have been in critical care it can take quite a while to get back to feeling your normal self, for some people this recovery can take up to one year. Recovery depends on the individual person and also many other factors, for example how long you were on the breathing machine, whether you have lost a lot of weight and whether you need to make any lifestyle changes.
These are some of the problems that patients may experience
| Fatigue | Loss of appetite |
| Anxiety | Weak voice |
| Depression | Breathing difficulties |
| Pain | Sleep disturbance |
| Swallowing difficulty | Social problems |
| Post-traumatic stress symptoms eg flashbacks, anxiety, fear, anger & jumpiness | Sensory changes including vision, hearing, taste & smell |
| Weakness | Difficulty walking or getting out of bed |
| Memory loss | Diarrhoea |
Sleeping
It is extremely common for patients who have been in intensive care to have problems sleeping. This is because their natural sleep pattern and body clock have been disrupted and it may take some time to get back to normal.
When your body is not active it does not need as much sleep, so as you increase your activity, you should find your sleep pattern returns to normal. You may find that a bath or shower shortly before going to bed will help you to feel relaxed, making it easier to sleep. Practising relaxation will also help. If you find you are sleeping a lot during the day, make a conscious effort to stay awake and your night time sleep should then start to improve. However, some people may need a short sleep in the afternoon, especially if that was your usual routine before coming into hospital.
Many people find that a bedtime drink is helpful but you should avoid caffeinated tea, coffee and large amounts of alcohol. Reading just before going to sleep is also a good way of relaxing. You can find yourself getting more worried at night; things easily seem to get out of proportion. It is common for a small problem to seem unsolvable in the early hours when you are the only person awake. This is quite normal, but when you have been ill it is often harder to cope with things like this.
You may find it helpful to read or listen to music if you are awake at night, they may help you go to sleep. Finally, the most important thing is not to worry about a lack of sleep, it won’t actually do you any harm and as you recover things will get backto normal.
Vivid dreams and delirium
Some patients experience very vivid dreams whilst in the critical care department or when they first leave. They may seem very real and frightening. They usually subside over a few days or weeks, it is common to experience this. Similarly some patients experience hallucinations or feelings that someone was trying to hurt them while they were in critical care. Again these memories are common, they are caused by a combination of being extremely unwell, the different environment and the drugs which are given to keep you comfortable.
This experience is called delirium and is very common in hospital. The staff in the hospital are used to looking after people who are not themselves due to delirium therefore it is not anything to be embarrassed about.
If you have had or are having problems like this it is important not to keep it to yourself. You may find it helpful to talk to a family member or to write the memories down. If the memories or dreams continue to trouble you it is important to talk to a member of the critical care team.
Changes in Mood
Remember, critical illness is an extremely stressful event; many people describe it as ‘life changing’. It is normal to have ‘good days’ and ‘not so good days’ throughout the recovery phase, which may include becoming angry, irritable and even tearful for no apparent reason.
Knowing this won’t make the problem go away but perhaps it will be easier to bear. If you have been very seriously ill or ill for a long time, you may find that you are quite low in mood at times. Like the other problems we have described this will go away and only rarely does it require special treatment.
Anxiety
It is normal to worry after being critically ill. Obtaining more information about worry or anxiety can help many people to handle it better. When we are worried, scared, in danger or under stress our bodies automatically produce chemicals to help us cope. The main chemical involved is adrenaline. In a real emergency it can help to save our lives.
Frightening events, words, thoughts or memories that you may have from critical care will cause the body to produce adrenaline. There is nothing wrong with this as it is part of nature’s way of helping you to cope with danger and live to fight another day. If we are in real danger we run or fight and so we don’t notice the effects it has on our body. The problems start when we have a worrying thought but can’t run away. The adrenaline gets our body ready in the same way as above, but as we aren’t running or fighting it doesn’t get used up and it causes unpleasant physical and mental symptoms.
Signs and Symptoms of Anxiety
Anxiety can-
- Make your thoughts race, so you can’t relax, or it may make getting to sleep difficult.
- Increase your breathing rate – this floods your brain with oxygen, making you feel dizzy or faint and far away.
- Speed up your heart rate – you may notice that your heart is racing or pounding.
- Shut down the stomach, giving you a feeling of butterflies or a sinking feeling
- Shut down the blood supply to your hands and feet – you may notice that they feel cold and clammy.
- Produce an unpleasant cold sweat – it may make your forehead feel clammy.
If you are suffering any of these symptoms it is important to discuss this with a family member or a health professional. For the majority of people, simply discussing thoughts and feelings help to alleviate the problem; rarely will it require specialist treatment.
The vicious cycle of anxiety

Depression
Low mood can be very common after being extremely ill. For most people these feelings usually go as time passes and they start to recover. However, people suffering from depression will experience a low mood and other symptoms each day for at least two weeks. Symptoms can become severe enough to interfere with day-to-day activities.
Signs and Symptoms of Depression
Depression can range from feeling sadness or tearful to absolute despair. It’s common to have several symptoms:
- Sadness
- Tearfulness
- Poor appetite
- Early waking
- Loss of interest in things that were once enjoyable
- Loss of interest in appearance
Most people with depression will get better without any treatment. However, this may take several months or even longer. Meanwhile living with depression can be difficult and distressing.
If you are suffering from any of these symptoms it is important to discuss this with your GP who can guide you towards one of the many treatment options available.
Diarrhoea
It is common for people to have diarrhoea on discharge from Critical Care and on discharge home. This may be due to change in diet and the medications you have received. It is important to continue to drink plenty of fluids when you experience this problem. It may subside after a few days but if you find this problem persists please seek advice from your GP.
Memory loss
You may find that you forget things more easily than before you came into hospital. This is quite common and should improve although sometimes memory is affected permanently. If you recognise this has happened do highlight this to your GP as there are treatments that can improve this.
Getting back to normal
Your body will have to do a lot of work to get back to normal, this will take time. There are several important things that you can do to help yourself recover.
Exercise
It is important that you undertake some exercise every day. Just walking up and down the stairs in your house every day will help. Going outside is very good for you, walking around the block or going somewhere you enjoy. Trying a little more every day will help you to see your improvement. Set small achievable goals, make a chart or use a calendar so you can see your improvement.
Exercise will keep your circulation active, help with muscle strengthening, build up your energy levels and help you to feel more positive.
Relaxation techniques
Relaxation can help in the following ways;
| Reduce stress | Reduce pain |
| Reduce fear and anxiety | Help with sleep |
| Coping with problems | Stop smoking |
| Help lower blood pressure | Reducing anger and irritability |
How to get started
Find somewhere quiet and warm. Make sure no one will interrupt you. Sit, or lie down somewhere comfortable. If you choose a chair to relax in make sure it is big enough to support your whole body, otherwise you won’t be able to relax. Allow yourself sufficient time (20-30 minutes). If you would like some quiet, gentle background music, that’s fine.
How to relax
Lightly close your eyes. Allow your breathing to slow and deepen. Imagine that you are in a place where you have always felt safe and calm. This might be on a beach in the warm sunshine, or in a hot bath. It is your personal place.
As you imagine your personal safe place, feel your body sinking into the chair or bed. Gradually relax all your muscles, starting at your feet and working up the body.
Be safe in the knowledge that no one can disturb you. Let go of all the physical tension in your body. Imagine peaceful, relaxing waves lapping round you taking the tension away.
Just breathe and relax, deeper and deeper with each slow and gentle out breath.
When you have spent a comfortable time feeling relaxed, bring yourself out of relaxation by counting slowly to five, becoming more aware of your surrounding. You will feel calm and ready to cope with anything.
If through the day you find yourself getting tense or anxious, take time to do a relaxation session. If you do not have time for that, bring the picture of your personal place into your mind and take some slow, deep breaths. Imagine in your mind the feeling of relaxation that you get from a full session and with practice you will be able to conjure up the feeling and so relax anywhere.
To start with, you will need to practice for about 20 minutes twice a day. At first you will need a quiet room to relax in, but as you become more experienced you will find you are able to shut out noise around you. Remember, eventually with practice, you will be able to relax anywhere.
Relaxation is not just beneficial for you. If you live with someone they may find that they also will benefit from learning how to relax. Get them to read this section and practice relaxation.
There are lots of videos on the internet to aid relaxation – type ‘relaxation techniques’ into www.youtube.com and you will find some guidance.
Eating Normally Again
At the beginning of your recovery it is common to notice that your eating habits and appetite might be different from before your hospital admission. Food may taste either slightly or dramatically different and some people are unable to taste anything at all. This is usually a temporary problem and will get better itself over time. However, it can be a problem as it may affect your appetite.
In addition to altered taste, many people find it difficult to manage their meal sizes especially if they have been artificially fed whilst in critical care. Initially, the amount of food the stomach can hold may be temporarily reduced and a feeling of fullness may develop even with modest portion sizes, it can also be quite tiring to eat.
Helpful tips
- Eat little and often – choose snacks high in protein and calories (such as cheese, mini pastries or ice cream) and milky drinks. Aim to have something small to eat every two or three hours.
- Take full advantage of times when you are hungry – have your favourite foods as often as you like and keep snacks handy to nibble on.
- Avoid very heavy, fatty foods if you find these hard to digest
- Avoid strong smelling foods if you are feeling sick. Instead choose cold options.
- If suffering with a dry or sore mouth, try having regular sips of milk or water and sucking on sugar free boiled sweets. If this is ineffective, visit your GP to discuss an artificial saliva spray or gel.
- Take your time – eat meals slowly and relax for a while afterwards
- If you feel full quickly, avoid liquids at meal times and have them later
It can take up to a year to get back to normal weight, and to reduce that extra fat and gain more muscle and it’s best to aim for slow and steady weight gain. If you have concerns that you continue to lose weight, help and support can be given from a member of the critical care team or for more specific advice referral can be made to a dietician.
Sex after Critical Illness
The old adage “a little of what you fancy does you good ” is particularly true for sex during your recovery from illness. Your illness may have reduced your sex drive and your partner may be concerned that sex could be harmful for you and indeed you may even feel that yourself. This is rarely the case but as with other forms of exercise, you should do as much as feels comfortable.
You will be able to return to your normal relationship but recognise that this may take some time and patience from both of you. A small number of people will have genuine medical problems – impotence for instance. If you require advice or support regarding these issues please talk to a member of the critical care team or your GP.
Lifestyle Changes
Smoking
If you smoked before your illness now is an ideal time to give up. If you stopped smoking while you were in hospital keep going now you are home. Smoking kills 100,000 people a year, it causes heart disease, strokes, bronchitis, emphysema, cancer, duodenal ulcers, sinusitis etc. Nicotine in cigarettes produces chemicals that make the heart work faster and so raises your blood pressure.
For patients who have been seriously ill in critical care it is important that they stop smoking. This is because the lungs are affected by the illness and can be damaged. People normally have a considerable amount of spare lung capacity so they do not notice the damage but it is important that you do not continue to damage your lungs after your illness by smoking and allow your lungs to recover. There is lots of free support available to you if you decide to stop smoking. The Tobacco Dependency Treatment Service QUIT Team provides an in house stop smoking programme for patients visitors and staff in Gateshead call them on 0191 4458963
Alcohol
Men should drink no more than 21 units of alcohol per week (and no more than four units in any one day). Women should drink no more than 14 units of alcohol per week (and no more than three units in any one day).
It is recommended that you have at least three days without alcohol a week. The more you drink above these limits, the greater the risk of developing serious problems, to find out more please speak to a health professional.
If you would like some help with this you can refer yourself to the alcohol team who will be happy to give you advice and support call them on 0191 445 3822
Support Services within the hospital
The Patient experience team provide:
- Advice and support for patients, their families and carers.
- Information on NHS services to help you make choices.
- Listening to your questions, suggestions, concerns and complaints
- Help sort out problems quickly on your behalf.
You can contact them at the Queen Elizabeth Hospital, Monday to Friday, 9am – 5pm call them on 0191 445 6129
Chaplaincy
The chaplains are here for all patients and relatives. Their work is to comfort the anxious and worried; to support people through difficult and stressful times; to provide spiritual support and to meet the religious needs of all within the hospital setting. They are here also to support relatives and they provide a safe and confidential setting for people to talk through their issues.
Chaplaincy can be contacted on 0191 445 2072
Part three – What to do once you go home
Going home is a big step after being in hospital and being so unwell but it is a very positive step. You and your family may feel anxious and that is very understandable.
The critical care rehabilitation nurse will telephone you once you are home to check how you are getting on and answer any queries you may have. You are free to contact the ward you were discharged from with any queries and also the critical care rehabilitation team on 0191 445 3210. If you would like to revisit critical care you are very welcome to arrange this with the critical care rehabilitation team.
If it has been deemed necessary you will be invited to a follow up appointment with the critical care rehabilitation nurse and a critical care physiotherapist a couple of months after you have been discharged home. This will be an opportunity for you to ask any questions and for the team to assess your progress. The team will also be able to guide you to community services which may be of benefit. People often find it reassuring to have this review as you may not realise for yourself the progress you have made since leaving hospital.
If you have not been contacted to arrange a review appointment please feel free to contact the rehabilitation team to arrange.
There is a local group called ICUsteps Gateshead which the rehabilitation team are involved with. They run very informal drop in meetings where you can meet people who have had similar experiences to yourself. Information on this group can be found on the next pages along with information about other organisations which you may find beneficial.
Useful telephone numbers
Your GP should be the first person you contact if you have concerns about your health but these numbers may also be useful.
Gateshead rapid response therapy team 0191 445 8400
Queen Elizabeth switchboard 0191 482 0000
Gateshead equipment services (for return of equipment) 0191 497 1599
Gateshead talking therapies (self-referral available) 0191 283 2541
For information about all services at QE Gateshead
National Support Groups and websites for information
ICUsteps Gateshead
ICUsteps is a national charity which was founded in 2005 by ex-patients, their relatives and ICU staff to support patients and their families through the long road to recovery from critical illness. ICUsteps stands for ‘Intensive care unit support team for ex-patients’.
The group provides peer support as you can meet people who have had similar experiences to yourselves as patients and relatives. The group is supported by the critical care rehabilitation team. There are social and fundraising events organised throughout the year. It would be lovely to see you there!
This group currently meets at Sherriff Hill Methodist Church on the last Thursday of the month from 1.30pm – 3.30pm. For more information see or ring the Critical Care Rehabilitation team on 0191 445 3210 or https://icusteps.org/support/support-groups/gateshead



Stopping Smoking
For free support, expert advice & tools including the Quit Kit to help you stop smoking call for free advice.
Free phone 0300 123 1044
Drugs
This site provides straightforward advice about drugs for young people.
Free phone 0800 77 66 00
Turning Point
Turning Point addresses the individual needs of people with substance misuse, mental health and learning disability. It is a leading social care organisation across England and Wales.
www.turning-point.co.uk
The Intensive Care Society (ICS)
The ICS is the organisation that represents medical healthcare professionals working in the field of critical care in the United Kingdom. The website has a patient and relatives area, information regarding meetings, guidelines and link to related critical care sites. www.ics.ac.uk
Health talk
The Health talk project is supported by the NHS and seeks to describe the patient experience using semi-structured interviews. The experiences of people who have experienced critical illness are available on the site. A must read! www.healthtalk.org
Alcoholics Anonymous
www.alcoholics-anonymous.org.uk
IF YOU HAVE A PROBLEM WITH ALCOHOL TEXT THE WORD HOPE TO 66777
If you want to contact the AA helpline for Tyne & Northumbria, the number is 0191 5214400
The national helpline number is 0800 9177650
Local meetings
Thursdays, St Peter’s Church, 21 Weathercock Lane, Low Fell, NE9 5JD
18.15 – duration 1hr
Thursdays, St Cuthbert’s Church, Shibdon Rd, NE21 5AE 19.00 – duration 1hr30mins
Meetings happening daily across Tyneside
An-Anon
For friends and relatives of people with alcohol dependency.
www.criticalcarerecovery.com
Useful website on recovering from critical illness
Local Support Services
Citizens advice Gateshead
0300 3309 035 citizensadvicegateshead.org.uk
For free, impartial advice on money, benefit, housing or employment issues.
Davidson Building, Swan Street, Gateshead. Speak to the Critical Care Rehab team if you need financial advice and they can arrange a fast track appointment.
Age UK Gateshead
0191 477 3559 www.ageuk.org.uk/gateshead/
Available for advice on benefits, day centres, group activities, gentle exercise and bereavement services.
Equal Arts
0191 261 1619 www.equalarts.org.uk
A creative ageing charity supporting older people in Newcastle, Gateshead and across the UK, working to improve the lives of older people through creativity and our arts activities around the North East.
Gateshead Carers Association
0191 490 0121 www.gatesheadcarers.com
Information and support service for those who care for people in Gateshead
British Red Cross
0191 273 7961 www.redcross.org.uk
Contact for short term wheelchair loan for £15 a week
Happy to Help
Community home help charity for older people and people with disabilities in Gateshead. £18.50/hr help with shopping/housework/ironing etc and one to one outing support.
Tyneside Women’s Health
0191 477 7898 www.tynesidewomenshealth.org.uk
Promoting positive mental health, well being and personal development of women through group activities including confidence building, anxiety management, skills development and varied activities groups.
Re-Co-Co Recovery College Collective
0191 261 0948 www.recoverycoco.com
Provide a peer led, peer delivered education and support service where people can learn from each other’s insights, skills and lived experience. Nurture a community of warriors and survivors towards a sense of belonging and acceptance for who, what and how they are.
Gateshead talking therapies
0191 283 2541 (ring to self-refer)
This team works with people who need support to get through times when they feel low, depressed or stressed. They run support groups, offer information classes and one to one therapy.
Gateshead Older People’s Assembly
0191 438 1721 www.gatesheadopa.ork.uk
A charity offering opportunities for Gateshead residents aged 50+ to maintain their independence and improve their mental and physical health.
Exercise classes from Go Easy Gateshead
Exercise classes led by staff who work with people who have long term conditions at Birtley, Dunston, Blaydon, Gateshead and Heworth leisure centres.
‘Move Easy’ for those looking for something very light, aims to improve strength, balance and flexibility, if you have a long-term condition or have been advised to take up gentle exercise this session is for you, combining seated exercise with an option to get up on your feet as your balance and strength improves. £2 per class. Contact Alyson or Sue to let them know you are attending.
Alyson Jordan covers Birtley, Heworth and Gateshead 07825 194251
Sue Robinson covers Blaydon and Dunston 07734 569799 [email protected]
| Venue | Day | Time | coach |
| Gateshead Leisure Centre | Monday & Friday | 11:00 – 11:45 | Alyson |
| Birtley Leisure centre | Wednesday | 11:00 – 11:45 | Alyson |
| Heworth Leisure centre | Tuesday | 11:00 – 11:45 | Alyson |
| Heworth Leisure centre | Thursday | 10:30 – 11:15 | Alyson |
| Dunston Leisure centre | Thursday | 10:30 – 11:15 | Sue |
| Blaydon Leisure centre | Tuesday | 11:45 – 12:30 | Sue |
| Blaydon Leisure centre | Wednesday | 11:00 – 11:45 | Sue |
Blue badge
If you normally use a car to get around you may be eligible for a ‘blue badge’ which allows you to park in disabled parking spaces. This can be applied for through Gateshead council either on their website or if you need a paper form call 0191 433 3636.
Exercise Plan
When you are getting ready to leave hospital the physiotherapist can provide you with advice on what exercise to do when you get home which will help you to recover quicker.
These are some suggestions which you can try depending on your ability.
Chair based exercise
The six rules of chair-based exercise
- Always use a strong chair, preferably with armrests and not too soft. When you sit in the chair, your thighs should be parallel with the floor. See exercise one.
- Keep your arm and leg movements steady, as this will help avoid muscle and joint strain. In the early stages, move your arms or legs one at a time. As you get more skillful, you can combine arm and leg movements in the same exercise. Ten to 12 repetitions per minute are normally enough, but you are the best judge of what you can manage.
- Warm up and cool down. When you start moving, the blood supply to the heart muscle needs a few minutes to reach optimal flow. Any combination of these exercises can be done gently to warm up or cool down, while you can do them more vigorously for the main part of your exercise session.
- Don’t exercise too hard. Aim for moderate-intensity exercise, which means you are slightly breathless and perhaps warmer than usual. Some days or weeks may be better than others, so adjust the intensity of the exercise to how you’re feeling.
- Never hold your breath while exercising. You’d be surprised just how often we forget to breathe when lifting our arms and legs or staying balanced.
- Keep your arm exercise below head height. This means the heart doesn’t have to pump so hard against gravity and will help to reduce breathlessness.
1. Alternate leg heel digs
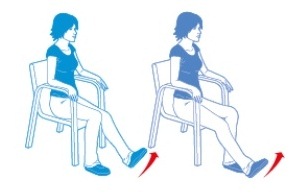
As one foot moves out to place the heel on the floor, the other foot remains planted on the ground. As the heel is placed on the ground, try to pull your toe towards your shin.
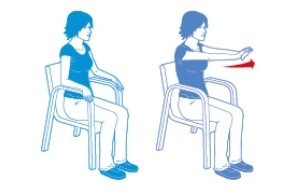
2. Alternate arm across body

Raise your right hand diagonally and touch your left shoulder. Return your right hand to the arm of the chair. Repeat motion, this time using your left hand to touch your right shoulder. Only reach as far across as is comfortable for you.
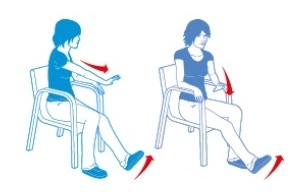
3. Double arm forward and back to the armrest
Push both hands forward to shoulder height. Your wrists should be extended. Coordination is important so, if possible, try to alternate which hand is in front of the other as your arms are forward.
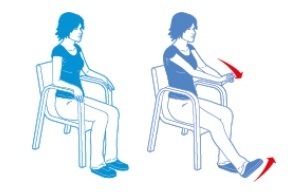
4. Alternate single arm across body with heel digs

Raise your right hand diagonally and touch your left shoulder. Simultaneously extend your left leg and plant heel on the ground. Return your right hand to the arm of the chair and your left leg to a relaxed position. Repeat motion, this time using your left hand to touch your right shoulder, while extending your right leg.
5. Alternate arm and leg
Push your leg forward and your opposite hand across your body, keeping your wrist extended. Your fingertips should be level with your shoulder. Only reach as far as is comfortable for you. With alternate arm and leg exercises such as this, it’s important that as one arm is moving, the other is supported on the chair, and the supporting foot is planted firmly on the floor.
6. Double arm forward with heel digs
Push your hands out slightly higher than your shoulder, in line with your chin, keeping your wrists extended. Only reach as far out as is comfortable for you. Coordination is important, so try to alternate which arm is in front of the other.
Acknowledgements: Nicky Cockerill and Nor Afifi Razaob
https://www.bhf.org.uk/heart-matters-magazine/activity/chair-based-exercises
General advice on 8 ways to get active every day
- Find an activity you enjoy and make it even more fun; listen to music while you do it or attend a class with a friend or family member.
- Everyday activity, such as walking or cycling to the shops or to work, is a great way to get your heart pumping. There is a greater chance of success if you build physical activity into your daily routine.
- If you enjoy walking, add some variety and push yourself further with Nordic walking poles. Using two poles while you walk gets your arms and core involved, making your physical activity more well-rounded.
- Use tools to support you, such as the NHS Choices’ Couch to 5k plan. Read about free apps for your smartphone that can inspire you to get active.
- Set yourself a goal or challenge. Why not take part in a mass participation challenge, such as a park run?
- Take advantage of the great outdoors – meet friends for a walk at your local park, or take your children or grandchildren for a kick-about.
- Encourage young children to be active through the games they play.
- Take the stairs instead of the lift or escalator, whenever possible.
More information see www.nhs.uk/better-health/get-active/
This is the aim in the long term!
Well done for getting to the end of the manual – hope you have found it helpful