This booklet is for patients who have had a Meniscus Repair at Gateshead Health NHS Foundation Trust.
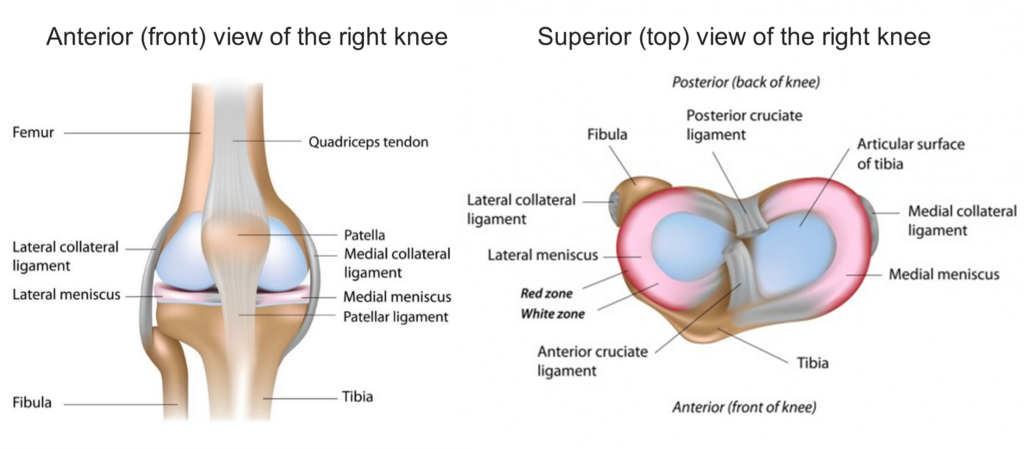
Anatomy
The meniscus is a ‘C’ shaped structure made of cartilage which sits between your tibia (shinbone) and your femur (thigh bone). There are two menisci in the knee, one on the inner (medial) side and one on the outer (lateral) side of the knee.
The meniscus works as a shock absorber and spreads the load on the surfaces of the knee.
What is a Meniscus repair?
A meniscus tear can be a result of an acute injury or degeneration. Acute injury may occur during activities that involve a forceful twisting motion. Some meniscus tears can heal without surgical management.
Some tears are not repairable, which will be determined by your consultant. The repair is dependent on the blood supply of the meniscus. Good blood supply allows for meniscal healing. To be repaired, the torn edges are stitched back into place.
Recovery after surgery
Goals of initial rehabilitation phase:
- Restore knee range of movement, especially being able to straighten the knee.
- Regain thigh strength
- Reduce swelling
- Adequate pain control
- Regain normal walking pattern.
Restrictions after surgery?
- Depending on your surgery you will initially have weight bearing and/or knee movement restrictions. This will be written on your front sheet of this leaflet by the physiotherapist.
- You will then need to avoid deep squatting until 12 weeks after your surgery.
- Initially you should not perform any twisting, turning or pivoting manoeuvres on your affected leg.
Discomfort
Post-operative pain, swelling, and bruising are a normal part of the recovery process. The muscles and tissues surrounding your knee will take time to heal. It is likely you will require pain relief medication on a reducing basis over several weeks following the surgery. Crutch use, ice, activity pacing and rest may help.
Following your discharge from hospital; you need to apply the ice pack three to four times daily for 15-20 minutes. You will be able to reduce the frequency after this time, but will find that you will benefit from ice therapy for up to three months to help manage the pain.
If you have any concerns regarding managing your pain, please discuss this with your GP.
Swelling
Swelling and inflammation is a normal part of the healing process. Dependant on your surgery this can last up to a few months. Swelling of the leg is different for everyone and may cause the leg to ache and feel very heavy.
Elevating your leg on a stool or on the bed will also help manage the swelling. Do not rest a pillow underneath your knee in a semi bent position. Although this may feel comfortable, it may cause problems with your movement and walking pattern.
If your leg suddenly becomes swollen, red, hot, painful or inflamed and you are unable to walk on your operated leg, call your GP as soon as possible. If your GP surgery is closed, go to your nearest A&E Department.
When should I seek help?
You should see your doctor urgently if you:
- Have a sudden increase in severe pain, swelling or tenderness in the calf which is getting worse and not just related to pain expected while performing the exercises.
- Have concerning pain, swelling or tenderness in the joint which is getting worse.
- Develop a persistent high temperature and feel generally unwell.
- See fluid, pus or blood coming from the wound.
Mobility and Walking aids
Your physiotherapist will provide you with a pair of crutches and show you how to use them. They will also complete a stair/ step assessment as required. Once you are no longer using your crutches; please return them to the hospital. You will be provided with further guidance from the outpatient physiotherapy staff as to when it is appropriate to gradually stop using elbow crutches.
If you do not have any mobility restrictions you must try to walk normally as soon as you can. However, it is important to avoid walking with a limp so you may need to use a stick or crutches initially to help you walk without a limp.
Stairs / Steps
if you are non-weight bearing your physiotherapist will show you how to complete the stairs safely
Going up stairs with a rail
Keep your crutch(es) on the step you are standing on.
Step up with your un-operated leg, then your operated leg and then bring your crutch(es) up onto the same step.

Going down stairs with a rail
Put your crutch(es) down first into the middle of the step below Step down with your operated leg and then follow by your un-operated leg.

Going up stairs without a rail
Keep your crutches on the step you are standing on.
Step up with your un-operated leg, then your operated leg and then bring your crutches up onto the same step.

Going down stairs without a rail
Put your crutches down first into the middle of the step below Step down with your operated leg and then follow by your un-operated leg.

Physiotherapy
It is important that you continue doing the exercises that have been given to you by the physiotherapist on the ward. These exercises should be completed three to four times a day.
It is normal to experience additional discomfort whilst doing these exercises and for up to an hour afterwards. Try taking your pain medication before exercising and using an ice pack afterwards.
Exercises
Lie on your back with your legs straight out in front of you:
Ankle pumps
Move your ankles up and down.
Repeat 10-20 times, 3-4 times a day

Heel Slides
Slide the heel of the operated leg along the floor and bend towards your buttock, trying to bend at your knee.
The physiotherapist on the ward would have explained and written on your front sheet of this leaflet what knee range of movement restrictions you have, do not exceed this range during this exercise.
Repeat 10 times, 3-4 times a day

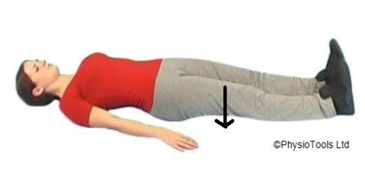
Thigh muscle (quadriceps) strengthening
Pulling your foot towards you and push your knee downward against the bed.
This exercise can be made easier by placing a rolled towel underneath your knee.
Hold for 5-10 seconds, Repeat 10 times, 3-4 times a day
End Range Knee extension
Place a rolled towel under your ankle. Straighten your knee by tightening your thigh muscle. Try to touch the bed with the back of your knee.
Hold for 5-10 seconds, Repeat 10 times, 3-4 time a day.

Outpatient physiotherapy
Once you have left hospital, you will receive outpatient physiotherapy rehabilitation. You should receive your appointments to attend outpatient physiotherapy via post after you leave hospital. This will be approximately two weeks after discharge.
If you are a registered patientof a Gateshead or Newcastle GP, the Tyneside Integrated Musculoskeletal Service (TIMS) will be your physiotherapy provider.
If you are a registered patient of Durham GP, the county Durham integrated MSK service will be your physiotherapy provider.
If you are an out of area resident (Registered to a GP out of Newcastle/Gateshead/Durham) the Queen Elizabeth Hospital will arrange your physiotherapy.
It is important that you attend outpatient physiotherapy. At this appointment the physiotherapist will:
- Assess the progress you have made since your discharge from the ward.
- Progress and guide on exercises.
- Assess your walking and progress to the most appropriate walking aid.
- Answer any queries you may have.
Follow up appointments will be arranged for physiotherapy at this appointment.
Please note: If you have not received notification of your follow up physiotherapy appointment/s within 2 weeks of leaving hospital, please ring 0191 445 2320 so we can check your referral.
On attending outpatient physiotherapy please wear clothing/ footwear that is suitable for exercise.
When can I return to exercise?
Returning to exercise timeframe will depend on your restrictions after surgery, you will begin with physiotherapy set exercises and you will be referred to outpatient physiotherapy. They will be able to progress your mobility and exercises to restore movement and strength. They will be able to guide you through your rehabilitation and explain when you are ready to progress to more advanced exercise and return to sports preparation.
Return to sport will depend on your progress you make with physiotherapy, therefore it is extremely important to attend your appointments and take on advice provided by them.
Work
You should return when you feel able to cope with the physical demands of your job. This will be sooner if you have a sedentary / desk based job. If you have a heavy manual job you may require up to 12 weeks off work. You can discuss this with your GP or Consultant if you are not sure.
Driving
If you have any restrictions you will be not be able to drive for at least 6 weeks following your operation. Once your restrictions have been removed and you are able to walk without any mobility aids you can drive when you feel safe to do an emergency stop and safely control the car. You must tell your insurance company that you have had knee surgery. If in doubt, contact your consultant or GP.
Telephone Numbers
If you are at all worried by your knee please contact us:
| During the hours of 8am – 8pm contact the Orthopaedic secretaries | 0191 445 8500 |
| During the hours of 8pm – 8am contact the Peter Smith Surgery Centre, Queen Elizabeth Hospital | 0191 445 2028 |
| During the hours of 0800 – 16:30 contact the Physiotherapy Department | 0191 445 2320 |
| During the hours of 8am-8pm. If you have a Gateshead or Newcastle GP, the TIMS will be your physiotherapy provider. If you have a query about your first appointment with TIMS please contact our booking team on 0191 445 2643 If you are a current TIMS patient and have a query about your follow-up appointment please contact our local admin team on 0191 213 8800 | Booking Team: 0191 445 2643 Local Admin Team: 0191 213 8800 https://www.tims.nhs.uk/ |
| During the hours of 8.30am-12pm and 1-4pm. If you have a Durham GP, the County Durham Integrated MSK Service will be your physiotherapy provider. | Central booking team: 01388 455 200 |
| Main Switchboard | 0191 482 0000 |