NHS funding for IVF has often been contentious. The North East however is the best area in England in terms of funding – offering 3 full cycles of treatment to eligible couples.
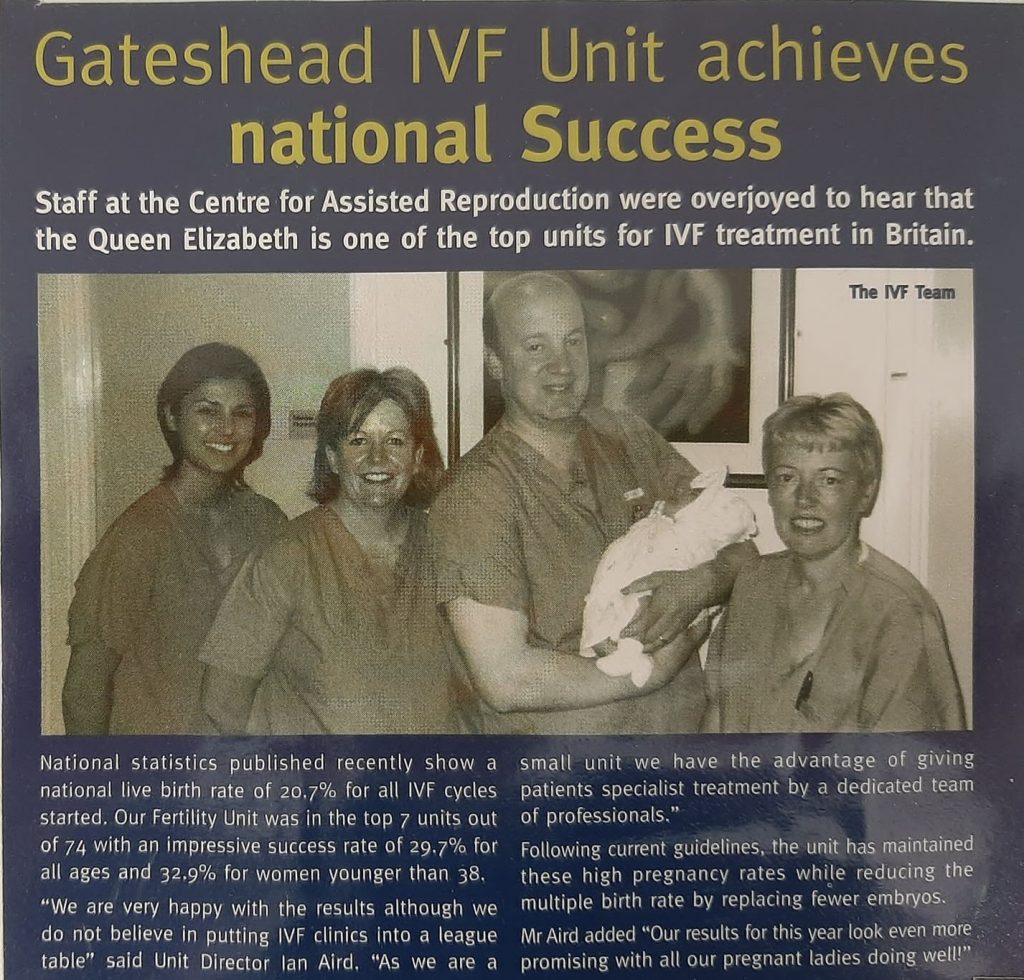
The IVF unit at Gateshead Health NHS Foundation Trust opened in 1997. Over the last two and a half decades, it has grown to be the largest provider of assisted conception in the North East and Cumbria and is rated among the highest performing IVF units by the Human Fertilisation and Embryology Authority (HFEA).
Fertility services in Gateshead started out small with a single full-time embryologist and two part-time nurses, a year later, Ian Aird was brought on board as a consultant. Initially, the unit was only performing 60 IVF cycles and a few insemination cycles per year.
“My time within the IVF department has been nothing short of exceptional and there have been many achievements over the years.”
Ian Aird Consultant in Obstetrics and Gynaecology and Fertility Services Lead at Gateshead Health NHS Foundation Trust.
The unit quickly grew and just three years after it opened, in 2000, it celebrated the birth of the 100th IVF baby.

In the same year, it introduced a new treatment called intracytoplasmic sperm injection (ICSI). ICSI was initially aimed at treating couples where the problem was related to the man’s sperm count. It involves injecting a single sperm onto the egg to assist fertilisation. This revolutionised the management of male factor infertility and was a major breakthrough in the field of assisted conception.
Over the next 10 years, the IVF unit in Gateshead continued to grow, with the appointment of new consultants as well as more nursing and laboratory staff. The number of cycles increased exponentially. Today the unit can perform over 500 cycles of IVF annually.
“During this time, we were consistently amongst the highest-performing IVF units in the country according to the success rates reported by the HFEA.”
Ian Aird
The original IVF unit was sited in maternity. It soon outgrew this tiny area and in 2009 moved to purpose-built premises on the third floor of the Jubilee Wing, which has the capacity to provide 500 cycles of IVF annually. In 2012, the unit celebrated the birth of the 1000th IVF baby.
Embracing new technologies
The department continued to embrace new developments and techniques. In 2015, it became the first trust in the region to offer time-lapse embryology to all IVF patients. This was a novel technique at the time. It allows the department to film the development of the embryo whilst in the incubator, by using time-lapse technology. The technology allows embryo development to be continuously monitored, without having to remove them from the stable environment of the incubator. It also allows for the manner of development of the embryo to be closely studied, which can help identify embryos with a higher implantation potential.
Around the same time as introducing the time-lapse technology, the unit introduced blastocyst culture, to allow this the unit had to be open six days a week. A blastocyst embryo is an embryo that is 5 days old. It has a higher chance of producing a pregnancy than a day 2 or day 3 embryo, which was the stage at which embryos had been transferred previously. This allows single embryos to be transferred more frequently, and results in a high pregnancy rate, while reducing the rate of more dangerous multiple pregnancies.
The unit has continued to grow, as well as performing up to 500 cycles of IVF using fresh embryos, it also performs 180 cycles using frozen embryos and 80 donor insemination cycles. It is one of the largest providers of assisted conception in the North East and Cumbria. To do this amount of work the IVF team has grown too. Currently, it has ten nursing staff, seven laboratory staff, three admin staff and five consultants who contribute to the assisted conception service.
“The strength of the unit is down to the efforts of the whole team. Without the huge efforts put in by my medical, nursing, laboratory and admin colleagues, we would not be in the great position that we are now.
“I would also like to recognise the support and guidance that we have received from the management team in the trust who have always been supportive when we have planned to introduce new developments to the service.
“As a team, we are also hugely appreciative of the support we receive from our patients largely through the fantastic feedback that we receive from them. Even during very difficult times, like during the pandemic, when we had to stop all treatments for three months, our patients, although disappointed that their treatment was delayed, were hugely supportive and respected the need for us to temporarily stop treatments.”
Ian Aird
Changing treatments
The biggest developments in the last 25 years include the introduction of ICSI, this really revolutionised the options available for cases of male factor infertility. For some couples, this meant there was a realistic chance that men with severe problems with sperm quality could have their own biological child. Prior to ICSI their only treatment option may have been to use donor sperm.
“The embryology developments that allowed growing embryos to be 5 days old (blastocyst stage) was also a big advancement as this allowed the selection of embryos with a higher implantation potential. This means we now normally only transfer a single embryo. By using blastocysts we still achieve high pregnancy rates, but we reduce the chance of a more dangerous multiple pregnancy. When I started IVF in the mid 1990’s, the norm was to transfer 3 embryos! “
Ian Aird
In the mid-1990s, pregnancy rates following IVF treatment were lower than they are now, but 25% of these were multiple. At Gateshead Health the current multiple pregnancy rate is around 5%.
“In recent years we are offering fertility treatments to a more diverse population allowing more couples to access treatment and experience parenthood and family life in a more modern setting.”
Ian Aird
The development of fertility treatments has always followed a pattern – to improve success rates and make treatments safer. There is a lot of research going on into reproduction and assisted conception to achieve these goals.
The main reason why IVF doesn’t work is that the embryos don’t stick when placed back in the womb. A lot of research is focussing on both the embryo and the womb to help identify healthy embryos with the highest implantation potential and also looking at the lining of the womb in an attempt to ensure it is in the most receptive state possible. This should lead to higher pregnancy rates, reduced rates of multiple pregnancies and fewer treatments required to achieve a healthy pregnancy.
“There are some fertility conditions that are difficult to treat, IVF obviously requires eggs and for some women who have low numbers of eggs or in women who are older there may be an egg quality issue, techniques to safely increase the numbers and quality of the eggs harvested could improve the treatment outcomes.”
Ian Aird
One of the more serious risks of ovarian stimulation during IVF is overproduction of eggs – ovarian hyperstimulation syndrome (OHSS). There is ongoing research looking at new drugs and new stimulation protocols to achieve the optimum ovarian response without increasing the risk of OHSS.
“Research into IVF and IVF itself has had its fair share of controversy in the past. Recent publicity regarding the creation of synthetic embryos is an example of this. This type of research needs close regulation, hence the need for organisations such as the HFEA that regulate all fertility treatments and research in the UK. It is sometimes difficult for the regulatory process to keep up with advances in assisted conception but this is essential to avoid abuse of the science.”
Ian Aird