This information pack includes the following:
- Service Details
- Referral Process
Guide for Referrers
This document introduces the clinical psychology services that form a part of Mental Health Services for Older People in Gateshead. It describes the service offered by clinical psychologists and the referral routes and criteria to access the service.
1. Background
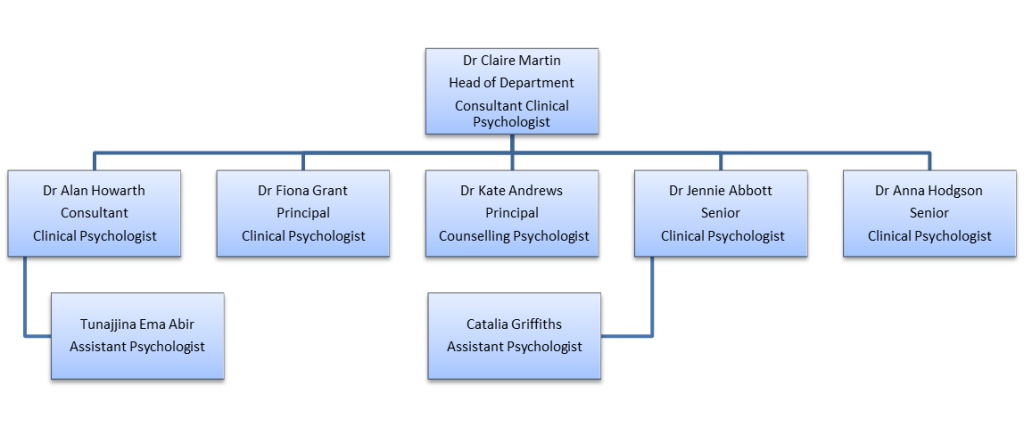
Clinical psychology services for older people in Gateshead have developed since 1988. There are now 5 clinical psychologists and 1 counselling psychologist totalling 5.5 wte staff.
Some clinical psychologists take doctoral trainees from the regional courses in Newcastle and Teesside for six-month clinical experience placements. At any one time there can be up to four trainee clinical psychologists working within the psychology department.
Assistant psychologists (pre-training) might also be a part of the psychology team. Their roles may vary, from service development and evaluation project work to supervised clinical work.
2. Parameters of the service
3. Service details
Clinical psychologists’ basic training involves completing a first degree in psychology followed by clinical and/or research assistant posts and then three years postgraduate doctoral training. Clinical psychologists working into mental health services for older people specialise in different aspects of psychological work with older people.
3.1 Direct clinical services
Clinical psychologists working with older people offer the following broad services:
- Assessment and formulation (a psychological explanation of the origin and maintenance of the problem)
- Psychological therapy (individual, couple, family or group)
- Neuropsychological assessment and post-diagnostic psychological support
Commonly referred psychological difficulties include:
- Memory problems
- Depression
- Anxiety and anxiety related difficulties e.g. Obsessive Compulsive Disorder
- Complex interpersonal and relationship problems
- Bereavement and loss
- Adjustment difficulties to physical health conditions e.g. stroke, Parkinson’s
- Behaviour that challenges in dementia
- Psychosis and delusional disorders
- Carer stress
Interventions
Generic
- Psychological therapy
- Patient and carer support, based on psychological formulation of need
- Indirect intervention, supporting and advising staff on issues relating to psychological aspects of a patient’s care. Indirect work will usually take place after the psychologist has directly assessed the identified patient.
- Education, training, supervision and consultation for colleagues in relation to psychological assessment, formulation and intervention.
- Formulation and reflection-based group supervision to help with understanding relational dynamics in the provision of mental health care, informing care plans and contributing to staff wellbeing (e.g. providing emotional scaffolding and avoiding burnout).
Specific psychological therapies currently offered within older people’s clinical psychology services include:
- Cognitive behavioural therapy (CBT)
- Cognitive analytic therapy (CAT)
- Compassion Focused Therapy
- Acceptance and Commitment Therapy (ACT)
- Eye Movement Desensitization and Reprocessing (EMDR)
- Systemic/family therapy
- Integrative therapy
NB. Not all clinical psychologists offer all forms of therapy
3.2 Assessment
Clinical
All referred patients will be directly assessed by the allocated psychologist. This includes patients referred for indirect work. Assessment will be completed using a range of methods, which may include:
- patient interview
- relative/carer interview where relevant
- standardised screening tools (e.g. measures of mood)
- behavioural observation (e.g. in care home settings)
- self-monitoring tasks.
A psychological formulation (see 3.1) will then inform any intervention offered to the patient/staff.
Neuropsychological
All psychologists currently take referrals for neuropsychological testing as part of the process of dementia diagnosis and care. It is useful for identifying detailed cognitive strengths and weaknesses, for cognitive rehabilitation and carer advice as well as providing differential diagnostic indicators (e.g. between depression and dementia; different dementia presentations; identifying at risk groups, such as those with mild cognitive impairment).
General indicators
- Basic cognitive screening (e.g. ACE-III) has not provided enough information to facilitate rehabilitation or carer support.
- Cognitive screening has not helped to identify cause of problems (differential diagnosis).
- The patient is in a high risk group (e.g. mild cognitive impairment) or is known to have a high premorbid IQ, and subtle cognitive change has been reported but not found by brief screening instruments (e.g. ACE-III) at rescreening.
Specific indicators
- Patient is willing to participate in cognitive assessment (3-4 hours total, spaced over several sessions)
- Patient is able to undergo cognitive assessment (physically, emotionally, practically)
Contraindications for Neuropsychological Assessment
- If neuropsychological assessment would not add to the care, diagnostic understanding or advice to patient/carer regarding presenting problems.
- If patient does not consent to undergo neuropsychological assessment, or (if unable to consent) if it would not be in the patient’s best interests to be assessed.
Criteria for Neuropsychological Retesting
Retesting would be helpful when:
- A diagnosis of mild cognitive impairment was the outcome of initial neuropsychological testing, and retesting (at 9 – 12 months) might assist diagnostic clarification.
- A recent significant change has occurred in the patient’s cognitive presentation and the nature of the difficulties remains unclear.
- Retesting is likely to add to the care of the patient (e.g. where an up-to-date cognitive profile will assist rehabilitation)
3.3 Therapy
Potential indicators for referral may include (but are not limited to):
- If the patient requests a referral to talk about their problems
- When there is evidence of some subjective patient distress regarding their situation or mental health
- Where the psychological nature of the patient’s presenting difficulties are evident to the referrer but not to the patient (e.g. interpersonal difficulties)
- When the patient wants to change their situation
- When staff in a care team (e.g. inpatient setting) are finding that the patient is difficult to care for or appears to be worsening in their mental health
- When a need for specialist psychology assessment has been identified within the team as a means of aiding problem formulation, staff care practice or to forecast likely benefit from psychological intervention.
- When there is a complexity or severity of the presenting problems and underlying factors that might be helped with a psychological understanding
4. Referrals
4.1 Referral criteria
- Person must be registered with a Gateshead GP (unless they are an inpatient).
- People aged 65+ (including carers) who are experiencing significant* mental health difficulties that require specialist psychological assessment, formulation and/or treatment that cannot be provided by any other service.
- People aged 65+ with significant* mental health difficulties associated with physical health comorbidities and/or frailty.
- Neuropsychological assessment (when required) for people currently under assessment for potential degenerative cognitive impairment (e.g. dementia).
There might be some circumstances where the above criteria apply to people under the age of 65. Examples include;
- Neuropsychological assessment to assist diagnosis of early-onset dementia.
- Patients under the age of 65 who have experienced a stroke and are currently an inpatient at the QE
- Carers of people with dementia who are open to the Mental Health Service for Older People.
If you are considering referring someone under the age of 65, please contact the department to discuss the appropriateness of the referral.
* Significant difficulties would be expected to result in considerable interference with relationships and/or social, occupational or other important areas of functioning [ICD-10].
The psychology service will decide about the appropriateness of each referral. If in doubt, patients will be assessed. Patients will only be directed elsewhere without being seen if there are exceptional circumstances e.g. if they live in the catchment area of another service.
4.2 Referral protocol
Refer to central point:
- referral form completed and sent via EMIS task to PsychologyAdmin inbox
- letter or email if the referrer does not have access to EMIS
- self-referrals can be made via telephone
4.3 Procedures on receipt referrals
- Each referral will be logged by the psychology admin team
- The referrals will be placed on our database to be discussed in the weekly allocation meeting.
- At this stage, referrals will either be accepted, rejected, or followed up if additional information is required.
- Once accepted, patients are put on the waiting list until they are allocated to a psychologist and an initial appointment can be offered.
- Service is directed towards those in the greatest need balanced by the likelihood of intervention being helpful.
Initial appointments
- The patient will be sent a letter offering either a clinic or a home appointment at the discretion of the psychologist and a copy of this letter will be uploaded on EMIS, or sent to the referrer (if no EMIS access).
Non attendance
- If the patient does not attend for their initial appointment, a further appointment will be sent.
- If the patient subsequently does not attend, further appointments will only be sent at the discretion of the psychologist, on a case-by-case basis.
- For patients on CPA, the clinician will notify the care co-ordinator to enable any necessary action to be taken
5. Communication with patient and referrers
Patients will be sent a letter:
- When they are placed on the waiting list
- When they have been allocated to a clinician, and therefore offered an initial assessment appointment
- Following an assessment (or after 5 consultations, whichever is sooner). This letter will consist of their psychology care plan. This letter will only be sent to the patient if they have consented to receiving it.
- Upon completion of therapy/psychological involvement. This letter will consist of the assessment summary, and if provided, intervention summary. Again, this letter will only be sent to the patient if they have consented to receiving it.
All letters mentioned above will also be copied to the referrers and uploaded onto EMIS (patients are able to choose whether they want the documents locked from non-mental health professionals).
6. Waiting list management
The aim of the service is to work at the timescale needed to effectively deliver psychological assessment and interventions that will influence patients’ wellbeing and recovery. Some patients may require priority over others, for instance; a patient within an acute ward with high risks may be seen before a patient who is due a routine reassessment. We aim to offer new referrals an initial assessment appointment within 28 working days; however, as mentioned above, if this is not possible then a waiting list letter will be sent to the patient. Following the initial assessment appointment, if appropriate, then intervention will be offered immediately as the service does not have a separate waiting list for treatment.